- Accidental Awareness During General Anaesthesia (AAGA)
- Awareness VIVA
- 1. Building Rapport & Setting the Scene (3 marks)
- 2. Information Gathering–Previous Event (3 marks)
- 3. Explains Nature of Prior Event (4 marks)
- 4. Discusses Awareness Under General Anaesthesia (3 marks)
- 5. Preventive Strategies for Upcoming Surgery (3 marks)
- 6. Communication Skills (4 marks)
- 7. Handles Patient Questions & Concerns (3 marks)
- 8. Structure & Professionalism (2 marks)
{}
Accidental Awareness During General Anaesthesia (AAGA)
Definition & Incidence
- AAGA: Explicit recall of intra-operative events under intended general anaesthesia—e.g., sounds, pressure, pain, paralysis.
- Incidence: Approximately 1:1,000 in structured studies like NAP5, ranging from 1:600 to 1:17,000 depending on methodology.
Sedation Depth Monitoring
| Technique | Pros | Cons |
|---|---|---|
| Autonomic/Somatic signs (BP, HR, tears) | Readily available | Low specificity |
| Movement/EMG | Simple | Blocked by NMB, not reliable |
| Isolated Forearm Technique | Detects consciousness during paralysis | Research tool only |
| Processed EEG (BIS, Entropy) | Quantifies sedation | Affected by EMG, NMB |
| Burst suppression | Indicates profound depth | Not protective from awareness |
- Key trial: BALANCE trial showed no mortality or major outcome differences by targeting BIS 50 vs 35—even though burst suppression depth varied.
Risk Factors for AAGA
- Emergency or obstetric procedures
- Rapid-sequence induction
- Use of neuromuscular blockers
- Obesity, difficult airway
- Interruption in anaesthetic delivery (e.g., during transport)
- Junior anaesthetist involvement
- Out-of-hours surgery
- Previous awareness
- Cardiac/thoracic surgery
- Young adult age (but not infants)
Clinical Evidence and Trials
| Trial | Design | Findings |
|---|---|---|
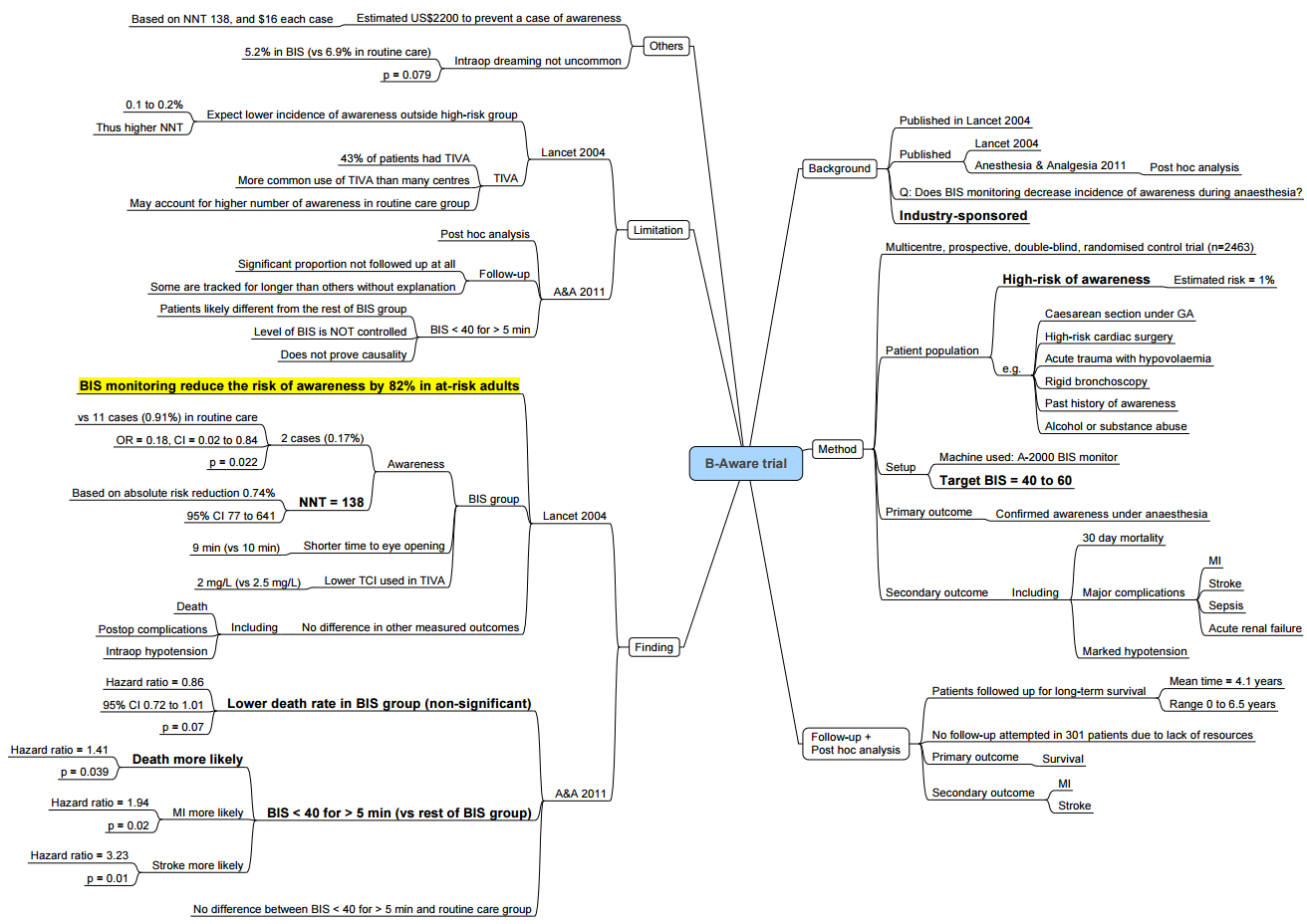
| B‑Aware (2004) | BIS 40–60 vs routine | Awareness 0.17% vs 0.91%; ARR 0.74%, NNT ≈ 697 |
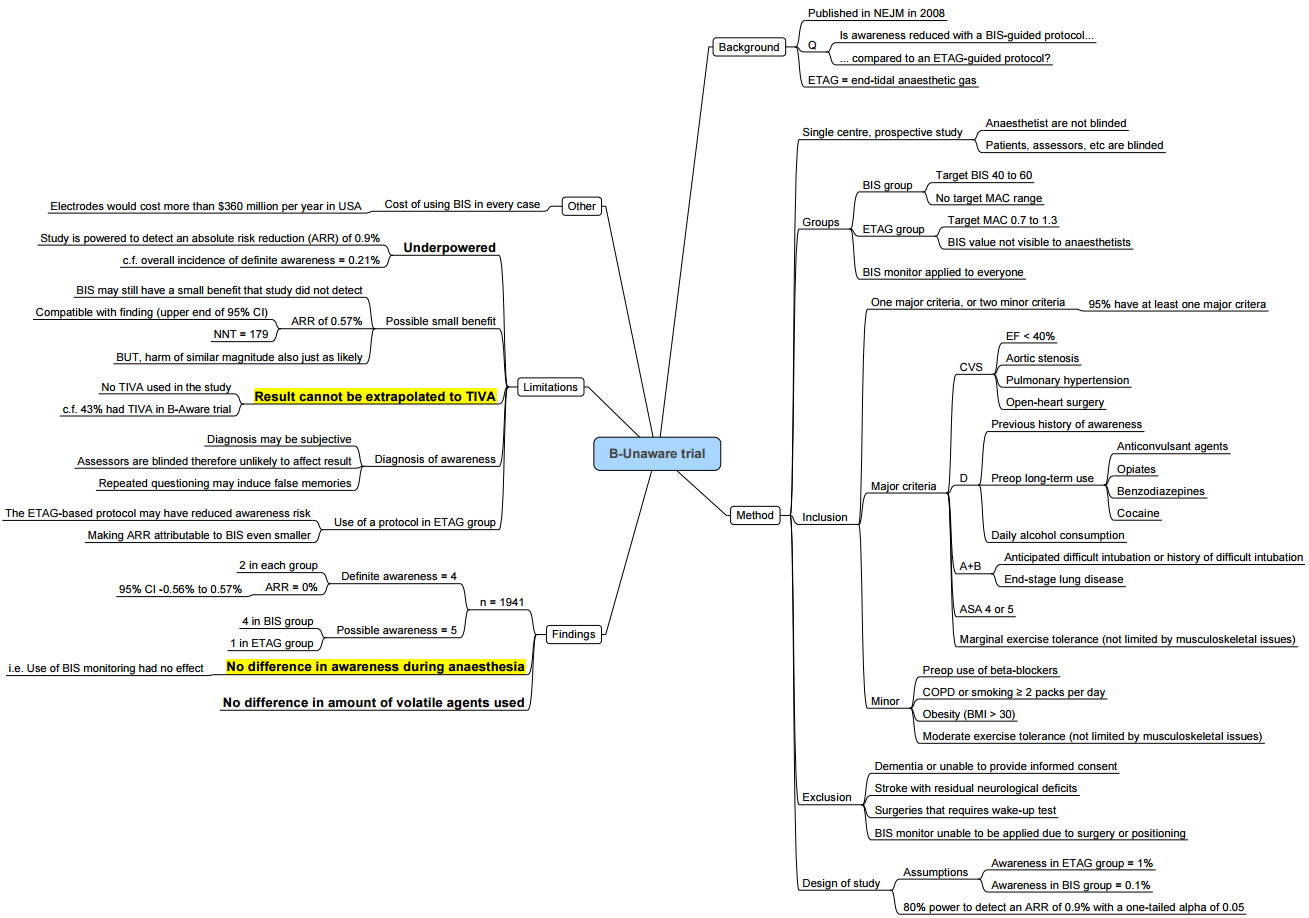
| B‑Unaware (2008) | BIS vs MAC-targeted volatile | No difference in awareness (0.21% both) |
| BAG‑RECALL (2011) | BIS vs MAC | No significant difference; BIS 0.28%, MAC 0.07% |
| MACS (2012) | BIS-guided vs routine care | No impact on awareness; trial stopped early |
| NAP5 (2014) | UK/Ireland survey | Overall incidence ~1:19,600; cardiothoracic procedures ~1:8,333; 41% had lasting psychological impact |
Prevention Strategy
Preoperative
- Identify high-risk groups
- Pre-op counselling with reassurance
- Premedicate (e.g., benzodiazepines) to reduce risk (not universally applied
Intraoperative
- Maintain age-adjusted MAC > 0.7
- Use processed EEG (BIS or entropy) for TIVA or NMB cases
- Monitor drug delivery and avoid interruptions
- Titrate NMB closely with objective monitoring
- Use infusion pumps with safety features
Postoperative
- Ask using the Modified Brice questionnaire in PACU and again within 24–72 hours
Management if Awareness Occurs
- Convene independent witness (colleague)
- Document event thoroughly
- Provide psychological support at 24 hours and 2 weeks; consider PTSD referral
- Report incident as a critical event
Patient Survey: Modified Brice Questions
- Last memory before sleep?
- First memory after waking?
- Any recollection during anaesthesia?
- Did you dream?
- Worst part of the experience?
- Helps distinguish awareness vs dreaming and assess patient distress.
Impacts of Awareness
- Short-term: anxiety, nightmares, flashbacks
- Long-term: PTSD, sleep disturbances, fear of future anaesthesia, medical avoidance
Clinical Recommendations
- Use depth-of-anaesthesia monitoring (BIS/entropy) in high-risk cases
- Keep volatile MAC ≥ 0.7 when used
- Ensure safe drug delivery—avoiding disconnections/delays
- Maintain vigilance during induction, emergence, transport phases
- Use postoperative screening (Brice tool) to detect and manage AAGA early
Awareness VIVA
Scenario: Counselling a patient with a past experience of awareness during a surgeon-led gastroscopy under midazolam, now scheduled for a laparoscopic cholecystectomy under general anaesthesia.
1. Building Rapport & Setting the Scene (3 marks)
- Greet the patient, introduce myself and my role as the anaesthetist.
- Explain: “I’d like to talk about your previous experience during your gastroscopy and discuss how we can minimise the risk of anything similar happening again.”
- Acknowledge their prior distress: “I understand that this was very distressing for you, and it’s completely reasonable to feel anxious before your next surgery.”
2. Information Gathering–Previous Event (3 marks)
- Use the Brice Questionnaire (or similar) to explore awareness:
- “What was the last thing you remember before going to sleep?”
- “What was the first thing you remember after waking?”
- “Do you remember anything in between?”
- “Did you have any dreams or sensations?”
- Clarify that the previous procedure was a surgeon-led gastroscopy using midazolam only, without an anaesthetist.
- Establish what they experienced (e.g., hearing voices, feeling discomfort, anxiety, partial recall).
3. Explains Nature of Prior Event (4 marks)
- Differentiate the event:
- “It sounds like your experience was due to inadequate sedation rather than true intraoperative awareness under general anaesthesia.”
- Explain contributing factors:
- “Midazolam causes sedation and some amnesia but doesn’t guarantee complete unconsciousness.”
- “Because there was no anaesthetist and the sedation may have been light, your awareness was not unexpected.
- Reassure:
- “You were not given any muscle relaxants or anaesthetic agents that cause full paralysis, so your safety wasn’t compromised in that regard.”
4. Discusses Awareness Under General Anaesthesia (3 marks)
- Define:
- “Awareness under general anaesthesia refers to a patient becoming conscious during surgery and having recall of events, which can be distressing.”
- Incidence
- “This occurs in about 1–2 cases per 1000 general anaesthetics.”
- Risk Factors:
- Previous awareness
- Equipment malfunction
- Emergency surgery
- Hypotension requiring lighter anaesthesia
- Elderly patients or those with altered physiology
- Acknowledge:
- “Having experienced awareness before slightly increases your risk, but we can take steps to greatly reduce it.”
5. Preventive Strategies for Upcoming Surgery (3 marks)
- Ensure continuous anaesthetist presence throughout the procedure.
- Use depth of anaesthesia monitoring (e.g., BIS or EEG-based monitoring) to titrate drug delivery.
- Conduct thorough equipment checks, ensure alarms are functioning, and confirm drug availability.
- Provide adequate analgesia and amnestic drugs.
- Arrange postoperative follow-up to address any concerns
6. Communication Skills (4 marks)
- Use open-ended questions: “How has this experience affected your confidence in undergoing surgery again?”
- Reflective listening and empathy: “It’s completely understandable to feel nervous—what you went through was very real.”
- Avoid minimising language (e.g., not saying “That’s rare, don’t worry”).
- Use simple language:
- “We’ll be closely watching your brain activity to ensure you’re deeply asleep.”
- Check understanding regularly: “Does that make sense so far? Any part you’d like me to explain more?”
7. Handles Patient Questions & Concerns (3 marks)
- “Will it happen again?”
- “The risk is low, and we are taking several steps to ensure it doesn’t.”
- “How will you know I’m asleep?”
- “We use monitors that assess depth of sleep and constant clinical observation.”
- “What if the equipment fails?”
- “We regularly test all equipment, and we have backups and alarms for every critical system.”
- Offer pre-medication (e.g., anxiolytics) or psychological support if desired.
- Acknowledge uncertainty when appropriate: “There is always a very small risk, but I’ll do everything I can to minimise it.”
- Offer further resources: “I can provide written information or refer you for a second opinion if you wish.”
8. Structure & Professionalism (2 marks)
- Logical and clear structure:
- Set the agenda → gather history → explain past → outline risks → propose strategy → answer concerns → summarise.
- Summarise:
- “To summarise: your previous experience was likely due to light sedation without anaesthetic drugs. Your upcoming surgery will be different—we’ll provide continuous monitoring, deeper anaesthesia, and post-op follow-up.”
- Invite further questions:
- “Do you have any other concerns you’d like to talk about?”
- Thank the patient for their time and openness.
BART
BE-UNAWARE
Links
References:
- Tasbihgou, S. R., Vogels, M. F., & Absalom, A. (2017). Accidental awareness during general anaesthesia–a narrative review. Anaesthesia, 73(1), 112-122. https://doi.org/10.1111/anae.14124
- Kim, M. C., Fricchione, G. L., & Akeju, O. (2021). Accidental awareness under general anaesthesia: incidence, risk factors, and psychological management. BJA Education, 21(4), 154-161. https://doi.org/10.1016/j.bjae.2020.12.001
- Pandit JJ, Cook TM, Jonker WR, et al. NAP5: Accidental awareness under general anaesthesia in the UK and Ireland. Anaesthesia. 2014;69(6):523–531.
- Myles PS, Leslie K, McNeil J, et al. BIS versus MAC for awareness prevention (BAG-RECALL). N Engl J Med. 2011;365(7):591–600.
- Avidan MS, Zhang L, Burnside BA, et al. Anesthesia awareness and BIS (B‑Aware). N Engl J Med. 2004;350:637–646.
- Monk TG, Saini V, Weldon BC, Sigl JC. Intraoperative Bispectral Index monitoring and awareness (B‑Unaware). Anesthesiology. 2008;109(3):613–620.
- Abend NS, Stain SC. PTSD after awareness under anesthesia. Anesthesiology. 2015;122(2):416–417.
- Bouafif‑Bossert MY, Bohnen NI. Depth of anesthesia monitoring: BIS and processed EEG in anaesthetic practice. BJA Educ. 2021;21(5):175–184.
- Everitt SJ, Management of intraoperative awareness. AAGBI Safety Guideline. 2020.
Copyright
© 2025 Francois Uys. All Rights Reserved.
id: “b01d6249-8cd2-40f1-bcf5-f10748ed4abf”



