{}
Summary of Amniotic Fluid Embolism
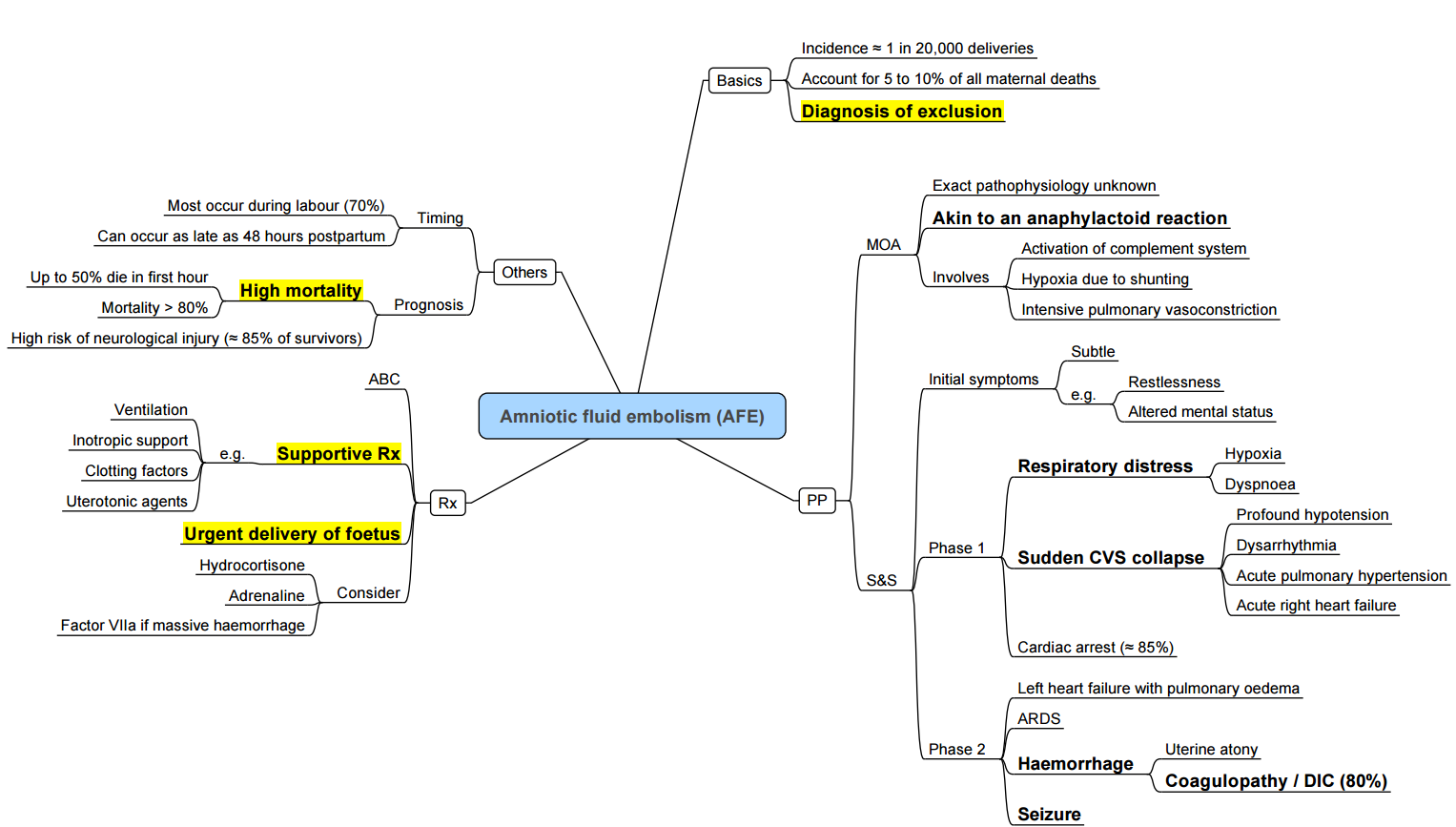
Amniotic Fluid Embolism (Safe)
Incidence and Mortality
- Incidence: Approximately 1.7–6.6 cases per 100 000 deliveries (≈1:20 000)
- Maternal mortality: 17–30%, with over 50% of deaths occurring within the first hour of presentation
Definition
Safe, also termed anaphylactoid syndrome of pregnancy, is a catastrophic obstetric emergency characterised by the sudden entry of amniotic fluid, fetal cells or debris into the maternal circulation, triggering pulmonary vasoconstriction, right ventricular failure, systemic hypotension and coagulopathy.
Pathophysiology
- Mechanical embolisation of particulate debris → pulmonary artery obstruction → acute pulmonary hypertension and right ventricular (RV) strain.
- Anaphylactoid reaction: release of arachidonic acid metabolites (leukotrienes, prostaglandins) → systemic vasodilatation, increased vascular permeability, pulmonary vasospasm.
- Coagulation activation: complement and tissue factor pathways → disseminated intravascular coagulation (DIC).
Clinical Presentation (Cardinal Signs)
- Sudden respiratory distress and hypoxaemia.
- Acute hypotension or cardiovascular collapse.
- Cyanosis and right heart failure (jugular venous distension, RV heave).
- Neurological compromise: seizures or coma.
- Coagulopathy: bleeding from puncture sites, oozing, prolonged PT/PTT, thrombocytopenia.
Diagnosis
- Clinical: abrupt onset during labour, delivery or within 30 min postpartum of respiratory and cardiovascular collapse with DIC, in absence of other causes
- Supporting tests: ABG (hypoxaemia, hypercapnia, metabolic acidosis), echocardiography (RV dilatation), standard coagulation panel.
- Definitive (post-mortem): fetal squames or hair in pulmonary microvasculature
Differential Diagnosis
| Obstetric Causes | Non‑obstetric Causes |
|---|---|
| Eclampsia | Pulmonary thromboembolism |
| Uterine rupture | Air/fat embolism |
| Placental abruption | Tension pneumothorax |
| Uterine inversion | Myocardial infarction |
| Peripartum cardiomyopathy | Anaphylaxis |
Management
Immediate Resuscitation (A–B–C)
- Airway and oxygenation: 100% O₂; early intubation and lung‑protective ventilation.
- Breathing: left uterine displacement to avoid aortocaval compression.
- Circulation: large‑bore IV access; rapid infusion of crystalloids; vasopressors (norepinephrine) and inotropes (dobutamine) to maintain MAP ≥ 65 mmHg.
- Perimortem caesarean: if cardiac arrest, deliver fetus by 5 min to improve maternal and fetal outcomes.
Haemorrhage and Coagulopathy
- Activate massive transfusion protocol: RBC:FFP:platelets 1:1:1 if DIC suspected.
- Cryoprecipitate and fibrinogen concentrate to maintain fibrinogen ≥ 2 g/L.
- Tranexamic acid 1 g IV; repeat once if bleeding continues.
- Consider recombinant factor VIIa only after correction of acidosis, hypothermia, thrombocytopenia.
Advanced Supportive Therapies
- Extracorporeal membrane oxygenation (ECMO) or RV assist device for refractory RV failure.
- Inhaled pulmonary vasodilators: nitric oxide, epoprostenol.
- Intra-aortic balloon pump (IABP) or cardiopulmonary bypass in extreme cases.
- Plasmapheresis: experimental to remove inflammatory mediators.
Maternal Pulmonary Embolism (PE)
Risk Factors
- Pregnancy‑induced hypercoagulability (↑ fibrinogen, ↓ protein S) and venous stasis.
- Personal or family history of VTE, inherited thrombophilia (Factor V Leiden, protein C/S deficiency).
- Obesity, advanced maternal age, immobility, caesarean section, pre‑eclampsia.
Clinical Presentation
- Sudden onset dyspnoea, pleuritic chest pain.
- Hypotension or shock (high‑risk PE) with RV dysfunction.
- Sudden decrease in end‑tidal CO₂ and oxygen saturation.
Diagnosis
- DVT evaluation: compression ultrasound of lower limbs.
- D‑dimer: elevated in pregnancy; normal value has limited negative predictive value, but a pregnancy‑adapted algorithm may be used.
- Imaging: ventilation–perfusion (V/Q) scan (low radiation) or CT pulmonary angiography (CTPA) if V/Q inconclusive or unavailable. ([
Prevention
- Perform VTE risk assessment in all pregnant women (RCOG Green‑top 37a).
- Pharmacoprophylaxis: LMWH for women at intermediate/high risk; mechanical methods (compression stockings, IPC) if anticoagulation contraindicated
Management
- Anticoagulation: therapeutic LMWH (e.g., enoxaparin 1 mg/kg q12h) adjusted to anti‑Xa levels; continue for ≥ 3 months and at least 6 weeks postpartum.
- High‑risk PE (shock or hypotension):
- Systemic thrombolysis (alteplase 100 mg over 2 h) unless contraindicated.
- Catheter‑directed thrombolysis or surgical embolectomy if thrombolysis contraindicated or failed.
- Refractory cases: ECMO as bridge to definitive therapy.
- IVC filter: reserved for contraindication to anticoagulation or recurrent PE despite anticoagulation.
Links
- Embolic phenomena
- Obstetric emergencies
- Maternal collapse and CPR
- Maternal conditions
- Venous air embolism
- Obstetrics Anticoagulation
Past Exam Questions
Amniotic Fluid Embolism
A 36-year-old woman in labour suddenly becomes “unstable” after 4 hours on an oxytocin infusion for poor progress.
a) What clinical features may lead you to suspect an amniotic fluid embolism? (5)
b) Give two differential diagnoses that may present with similar clinical features. (2)
c) What is the cardio-respiratory pathophysiology of amniotic fluid embolism? (3)
References:
- Allman K, Wilson I, O’Donnell A. Oxford Handbook of Anaesthesia. Vol. 4. Great Clarendon Street, Oxford, OX2 6DP, United Kingdom: Oxford University Press; 2016.
- Butterworth J, Mackey D, Wasnick J. Morgan and Mikhail’s Clinical Anesthesiology, 7th Edition. 7th edition. New York: McGraw Hill Medical; 2022.
- Bready L, Mullins R, Noorily S, Smith R. Decision Making in Anaesthesiology: An Algorithmic Approach. 3rd Edition. Maryland Heights, MO: Mosby Elsevier; 2007. pp 436-37.
- 1Clark SL, et al. Amniotic fluid embolism: analysis of the National Inpatient Sample. Am J Obstet Gynecol. 2021;225(1):59.e1–59.e7.
- Stafford I, Sheffield J. Amniotic fluid embolism. Obstet Gynecol Clin North Am. 2023;50(2):345–360.
- Kon nstantinides SV, et al. 2019 ESC guidelines for the diagnosis and management of acute pulmonary embolism. Eur Respir J. 2019;54(3):1901647.
- Bates SM, et al. American Society of Hematology 2018 guidelines for management of venous thromboembolism in pregnancy. Blood Adv. 2018;2(22):3317–3359.
- Royal College of Obstetricians and Gynaecologists. Green‑top Guideline No. 37a: Reducing the risk of VTE during pregnancy and puerperium. London: RCOG; 2015.
Summaries:
—
Copyright
© 2025 Francois Uys. All Rights Reserved.
id: “7045dc1f-2535-4b26-b904-69fa5982eccc”



