- Vaughan Williams Classification of Anti-arrhythmic Agents
- Mechanism of Action
- Normal Membrane Potentials
- Potassium and Sodium Movement
{}
Vaughan Williams Classification of Anti-arrhythmic Agents
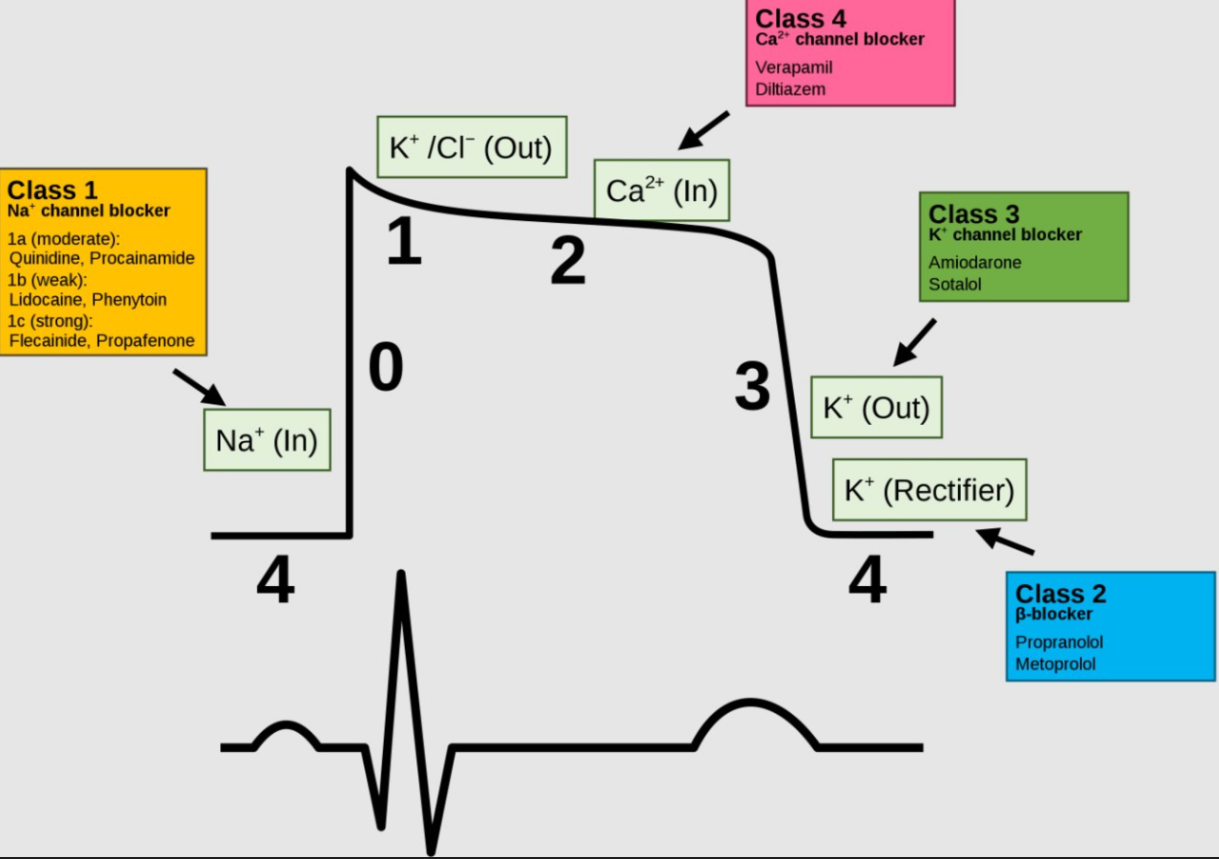
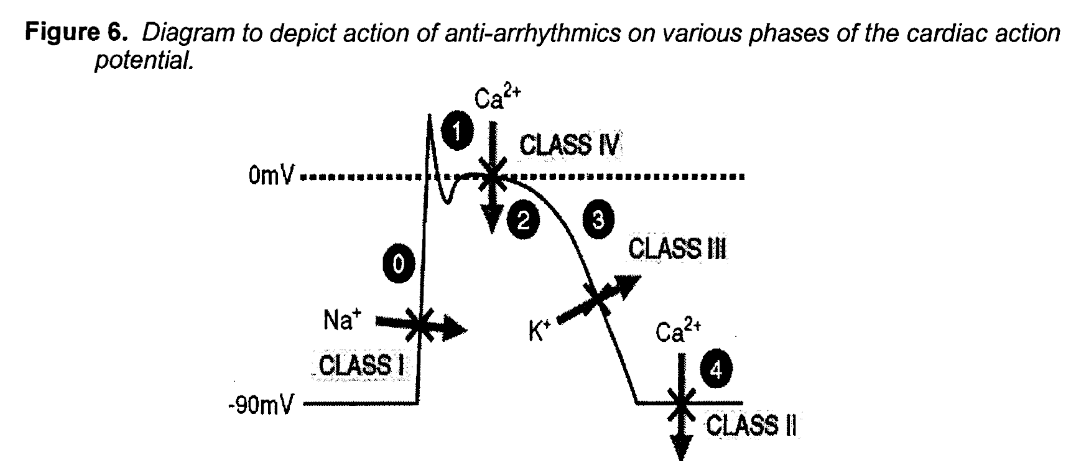
- The Vaughan Williams (VW) scheme groups drugs by the dominant ion-channel or autonomic effect on the cardiac action potential. Many modern agents display mixed properties, and newer drugs (e.g. ivabradine) lie outside the original four classes; nevertheless the VW system remains the core framework examined in specialist curricula.
| Class | Primary target | Effect on ECG | Representative drugs (RSA availability bold) | Typical indications | Key safety issues |
|---|---|---|---|---|---|
| I (Na⁺ block) | Fast Na⁺ channel | ↓ Phase 0 upstroke; QRS ± QT | Ia quinidine, procainamide, disopyramide • Ib lidocaine, mexiletine • Ic flecainide, propafenone | SVT & VT (Ic in structurally normal hearts; Ib for ischaemic VT) | Pro-arrhythmia (torsades with Ia, CAST mortality with Ic in IHD) |
| II (β-block) | β-adrenergic receptor | ↓ slope of phase 4; ↑ PR | Esmolol, atenolol, metoprolol, sotalol* | Rate control (AF), catechol-triggered VT, congenital long-QT | Bradycardia, bronchospasm, masking hypoglycaemia |
| III (K⁺ block) | I_Kr / I_Ks | QT prolongation; ↑ ERP | Amiodarone, dronedarone, sotalol, dofetilide, ibutilide* | Rhythm control (AF), VT suppression, WPW | Torsades (except amiodarone), extracardiac toxicity (amiodarone) |
| IV (Ca²⁺ block) | L-type Ca²⁺ channel | ↑ PR; little QT effect | Verapamil, diltiazem | AV-node dependent SVT, rate control of AF | Hypotension, worsened HF with LVSD |
| V (Misc.) | – | – | Adenosine, digoxin, magnesium, ivabradine | Diagnostic or rate-slowing (adenosine), rate control & inotropy (digoxin), torsades prophylaxis (Mg²⁺) | Drug-specific (see below) |
- _Sotalol combines non-selective β-blockade (Class II) with dose-dependent IKr inhibition (Class III).
Class I–Na⁺ Channel Blockers
Pharmacology
- Ia moderate Na⁺ block and I_Kr block → ↑ action potential duration (APD) & QT.
- Ib weak Na⁺ block; selective for depolarised/ischaemic tissue → ↓ APD.
- Ic strong Na⁺ block; minimal effect on repolarisation but marked QRS widening
Clinical Pearls
- Flecainide/propafenone effective “pill-in-the-pocket” cardioversion in paroxysmal AF with normal ventricles. Contra-indicated in coronary or structural heart disease (CAST).
- Lidocaine remains first-line for ischaemia-related VT/VF when amiodarone is unavailable or when ROSC is delayed; recent observational data suggest higher pre-hospital ROSC versus amiodarone.
- Procainamide IV favoured over amiodarone for stable monomorphic VT in 2022 ESC VA guideline (Class IIa)
Class II–β-Adrenergic Antagonists
- Reduce Ca²⁺ influx at the sinus and AV nodes, flatten phase 4 and prolong refractoriness, especially within ischaemic border zones.
- Robust outcome data: β-blockers reduce mortality post-MI and in heart failure, and lower sudden death risk in congenital long-QT.
- Esmolol (ultra-short acting) is useful for rapid peri-operative rate control.
- Sotalol needs in-hospital initiation (≥3 days) to monitor QTc; torsades risk rises sharply when creatinine clearance < 60 mL min⁻¹.
Class III–K⁺ Channel Blockers
Amiodarone
- Multi-channel blockade (I_Na, I_CaL, I_Kr, β-blockade) → minimal torsades risk despite marked QT.
- Extremely long half-life (15–60 days); load 5 mg kg⁻¹ over 1 h, then infusion 15 mg kg⁻¹ day⁻¹.
- Toxicities: pulmonary fibrosis, thyroid dysfunction (inhibits T4→T3 conversion), hepatotoxicity, corneal micro-deposits, photosensitivity.
Dronedarone
- Non-iodinated amiodarone analogue with shorter t½ (~24 h).
- Contra-indicated in NYHA III–IV HF or LVEF < 35 %.
- 2023 Veterans cohort: lower ventricular pro-arrhythmia and bradycardia than sotalol, with similar mortality.
Other Agents
- Dofetilide (not marketed in SA)–mandatory in-hospital loading; safe in LV dysfunction.
- Ibutilide–IV conversion of recent-onset AF/AFl; monitor for torsades.
- Bretylium is obsolete.
Class IV–Non-dihydropyridine Ca²⁺ Channel Blockers
- Slow AV nodal conduction and prolong node refractoriness.
- Useful for termination of AVNRT/AVRT and ventricular rate control in AF (when β-blockers contra-indicated).
- Avoid if LVEF < 40 % or concomitant β-blockade (heart block risk).
- Verapamil causes cerebral vasodilatation and is sometimes used in refractory cerebral vasospasm.
Class V–Miscellaneous / Unclassified
| Drug | Mechanism | Typical dose | Clinical notes |
|---|---|---|---|
| Adenosine | A₁-receptor → ↑ K⁺ outflow, ↓ cAMP | 6 mg rapid IV push (then 12 mg) | Diagnostic & therapeutic for AV-node dependent SVT; contra-indicated in asthma |
| Digoxin | Na⁺/K⁺-ATPase inhibition (↑ Ca²⁺) + vagotonic AV block | Load 10–15 µg kg⁻¹ PO/IV | Narrow therapeutic index; toxicity worsened by hypokalaemia & renal failure |
| Magnesium | Modulates Ca²⁺ influx, stabilises membrane | 2 g IV over 5 min | First-line for torsades de points even with normal Mg²⁺ |
| Ivabradine (Class 0) | Funny-current (I_f) inhibition | 5–7.5 mg PO bd | Lowers sinus rate without BP effect; benefit in inappropriate sinus tachycardia |
Guideline-directed Drug Selection (2020–2025)
- First-line rhythm control in AF (no structural heart disease): flecainide, propafenone, sotalol, dronedarone.
- Heart failure, significant LV hypertrophy or post-MI: amiodarone or dofetilide preferred; avoid Ic agents.
- Stable monomorphic VT: procainamide > amiodarone > sotalol (ESC 2022).
- Polymorphic VT / torsades: cease QT-prolonging agents, give Mg²⁺ 2 g IV, correct K⁺ > 4.5 mmol L⁻¹, institute over-drive pacing.
Mechanism of Action
Action Potentials and Ion Concentrations in Neuronal and Cardiac Tissues
Action Potential in Neuronal Tissue
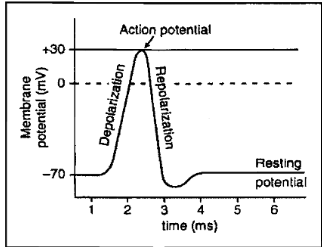
- Depolarisation: Opening of sodium channels allows sodium ions to enter the neuron, causing the membrane potential to become more positive.
- Repolarisation: The positive membrane potential stimulates the opening of potassium channels, allowing potassium to leave the neuron, resulting in a small overshoot before returning to resting potential.
Figure 2: Action Potential in Cardiac Myocytes
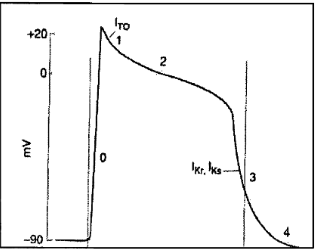
- Phase 0: Voltage-gated Na⁺ channels open, and Na⁺ enters the cell.
- Phase 1: Initial rapid repolarisation as Na⁺ channels close.
- Phase 2: Slower, prolonged opening of voltage-gated Ca²⁺ channels.
- Phase 3: Closure of Ca²⁺ channels and K⁺ efflux.
- Phase 4: Cell membrane becomes permeable to K⁺ ions but remains relatively impermeable to other ions.
Normal Membrane Potentials
Steady State Distribution of Ions in the Intraand Extracellular Compartments of Cardiac Myocytes
| Ion | Extracellular Concentration (mmol/L) | Intracellular Concentration (mmol/L) |
|---|---|---|
| Na⁺ | 135-145 | 10 |
| K⁺ | 3.5-5.0 | 155 |
| Cl⁻ | 95-110 | 20-30 |
| Ca²⁺ | 2 | 10⁻⁴ |
Diagram of the Membrane Potential for Pacemaker Tissue
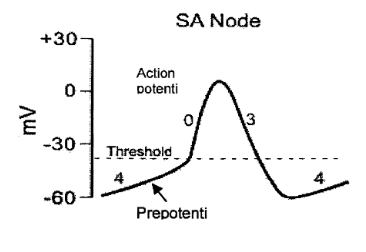
- Pre-Potential: The pre/pacemaker potential triggers the next impulse. At the peak of each impulse, K⁺ efflux causes repolarisation. As K⁺ efflux slows, the membrane begins to depolarise, forming the first part of the prepotential.
- Calcium Channels: Initially, T-type (transient) calcium channels open, completing the pre-potential. This is followed by the opening of L-type (long-lasting) calcium channels, producing the impulse.
Potassium and Sodium Movement
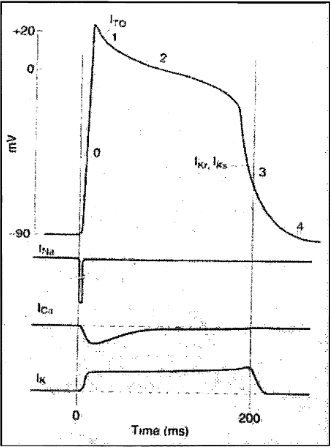
Phases of Cardiac Action Potential
-
Phase 0 (Depolarization)
- Ionic Movement: Rapid influx of Na⁺ ions through voltage-gated Na⁺ channels (I_Na).
- Voltage Change: Rapid rise in membrane potential from -90 mV to approximately +20 mV.
-
Phase 1 (Initial Repolarization)
- Ionic Movement: Transient outward K⁺ current (I_to) briefly flows out of the cell.
- Voltage Change: Slight decrease in membrane potential following the peak of depolarization.
-
Phase 2 (Plateau Phase)
- Ionic Movement: Slow influx of Ca²⁺ ions through voltage-gated Ca²⁺ channels (I_CaL) balanced by K⁺ efflux (I_Kr, I_Ks).
- Voltage Change: Membrane potential remains relatively stable, forming a plateau.
-
Phase 3 (Repolarization)
- Ionic Movement: Continued efflux of K⁺ ions through delayed rectifier K⁺ channels (I_Kr, I_Ks).
- Voltage Change: Gradual return of the membrane potential towards the resting level.
-
Phase 4 (Resting Membrane Potential)
- Ionic Movement: Maintenance of the resting membrane potential primarily by K⁺ currents.
- Voltage Change: Membrane potential stabilizes at around -90 mV.
Ionic Currents
- I_Na (Sodium Current): Responsible for the rapid depolarization during phase 0.
- I_to (Transient Outward Potassium Current): Contributes to the initial repolarization in phase 1.
- I_CaL (L-type Calcium Current): Maintains the plateau phase during phase 2 by allowing a slow influx of Ca²⁺.
- I_Kr, I_Ks (Delayed Rectifier Potassium Currents): Facilitate repolarization during phase 3 by allowing K⁺ efflux.
Drugs Targeting Site
Links
References:
- Hindricks G, Potpara T, Dagres N, et al. 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation. Eur Heart J. 2020;41:373-498. escardio.org
- Zeppenfeld K, Tfelt-Hansen J, de Riva M, et al. 2022 ESC Guidelines for ventricular arrhythmias and prevention of sudden cardiac death. Eur Heart J. 2022;43:3997-4126. pubmed.ncbi.nlm.nih.gov
- King GS, Goyal A, Grigorova Y, et al. Antiarrhythmic Medications. StatPearls (updated Feb 2024). ncbi.nlm.nih.gov
- Pundi KN, Kabadi AM, Blomström-Lundqvist C, et al. Dronedarone versus sotalol in antiarrhythmic drug-naïve veterans with atrial fibrillation. Circulation Arrhythm Electrophysiol. 2023;16:e011893. pubmed.ncbi.nlm.nih.gov
- American College of Cardiology/American Heart Association/Heart Rhythm Society. 2023 ACC/AHA/ACCP/HRS Guideline for the diagnosis and management of atrial fibrillation. Circulation. 2024;149:e936-e995. pubmed.ncbi.nlm.nih.gov
- FRCA Mind Maps. (2024). Retrieved June 5, 2024, from https://www.frcamindmaps.org/
- Anesthesia Considerations. (2024). Retrieved June 5, 2024, from https://www.anesthesiaconsiderations.com/
- ICU One Pager. (2024). Retrieved June 5, 2024, from https://onepagericu.com/
Summaries:
Anti-arrythmatics
Copyright
© 2025 Francois Uys. All Rights Reserved.
id: “bef30fb0-ed83-42dd-98d7-ca9d9f869813”



