{}
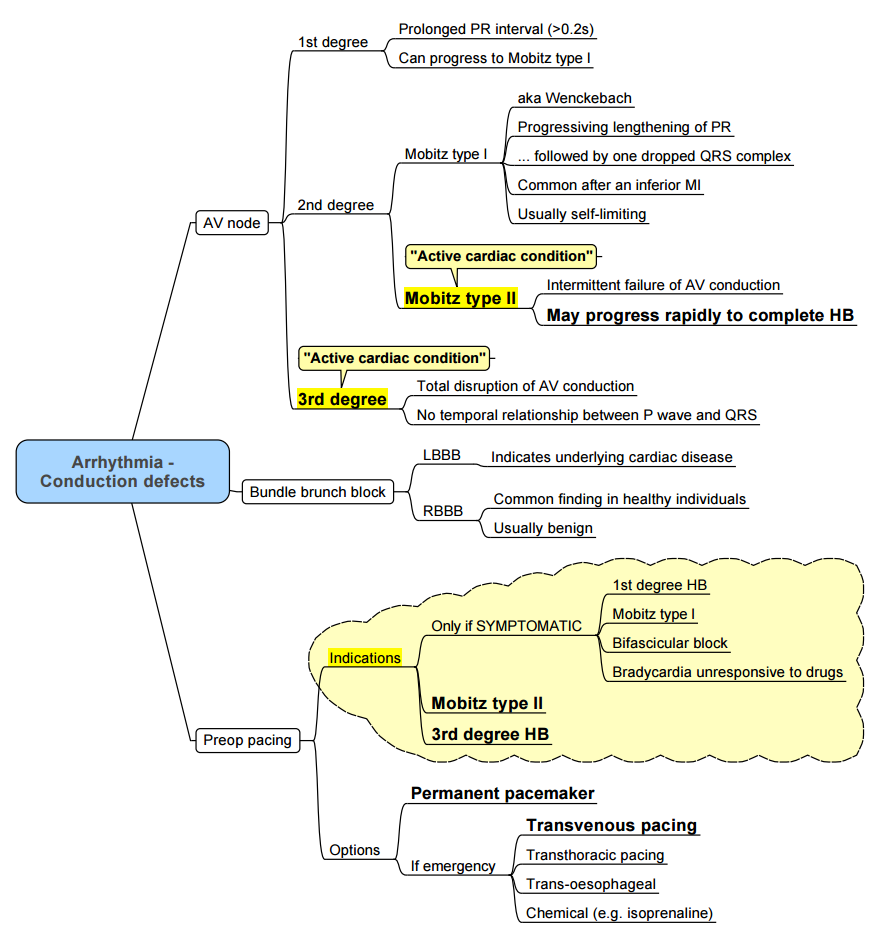
Approach to Any Arrythmia
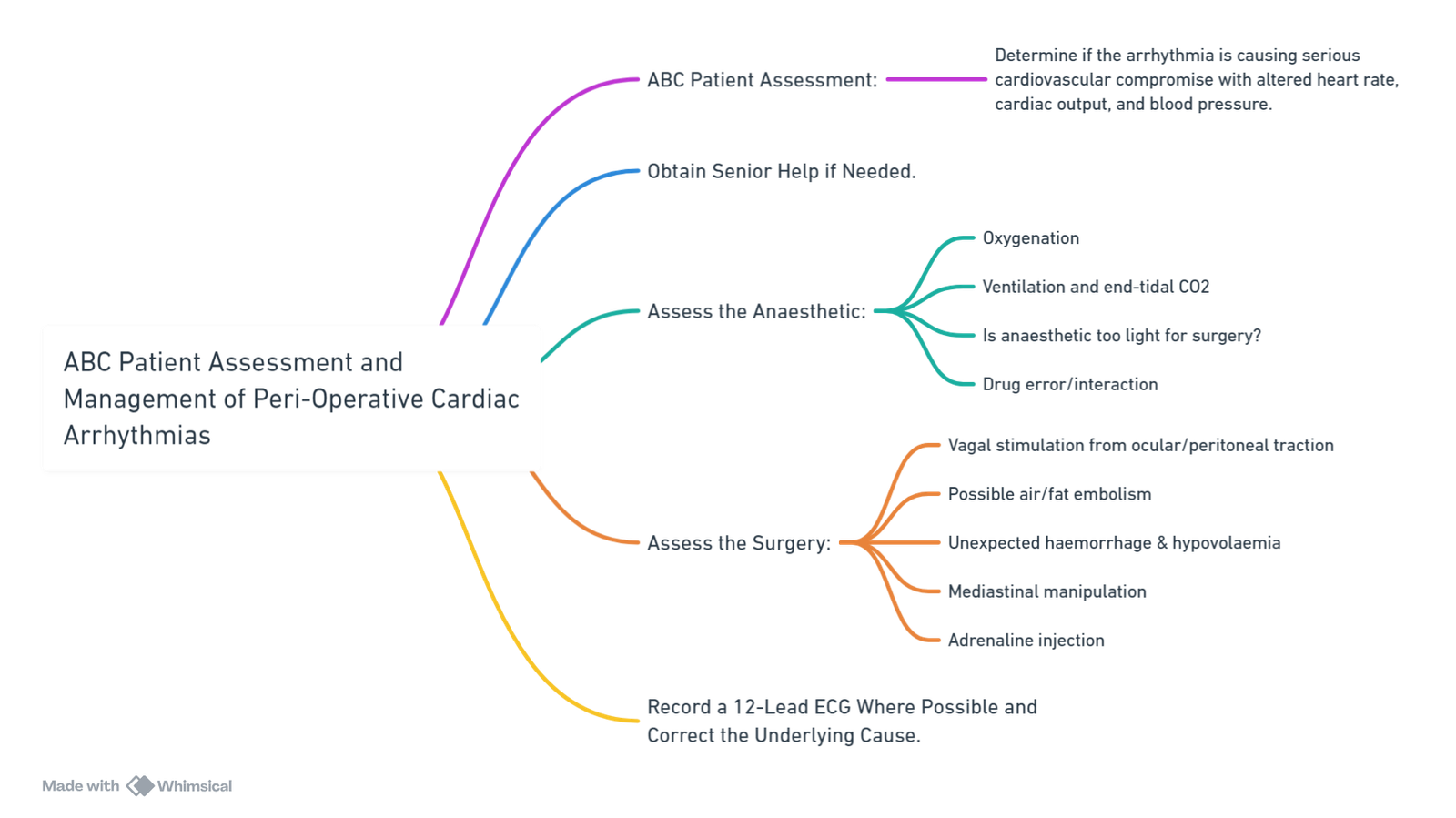
ABC Patient Assessment and Management of Peri-Operative Cardiac Arrhythmias
Tachyarrhythmias
A Simple Approach to Tachyarrhythmias
Regular, Narrow Complex
- Sinus tachycardia
- Ectopic atrial tachycardia
- Atrial flutter
- AV nodal re-entry (AVNRT)
- AV re-entry (AVRT)
Irregular, Narrow Complex
- Atrial fibrillation (AF)
- Atrial flutter with variable block
- Multifocal atrial tachycardia (MAT)
Regular, Broad Complex
- Ventricular tachycardia
- SVT with bundle-branch block
- SVT with aberrant conduction
- SVT with eccentric conduction
- Ventricular pacemaker
Irregular, Broad Complex
- AF with bundle-branch block
- AF with aberrant conduction
- AF with eccentric conduction
- Multifocal ventricular rhythm
- Torsade de Points
Monomorphic VT
Definition:
- A wide QRS complex tachycardia originating from the ventricles lasting > 30 seconds. Mechanisms include re-entry (e.g., scar-mediated) or increased automaticity.
Pathophysiology:
- The sinoatrial node continues to depolarize the atria while the ventricles depolarize independently.
- Re-entrant circuits or ectopic focus uniformly depolarize ventricular myocytes.
Mechanism and Symptoms:
- Heart Rate > 100 beats/minute: Decreased ventricular filling time, preload, and stroke volume, leading to palpitations and hypotension.
- Right Atrium: Contracts against a closed tricuspid valve causing Cannon A waves.
ECG Findings:
- AV dissociation
- Uniform morphology of QRS complexes
- Wide QRS complexes (≥ 120 milliseconds)
Complications:
- Inadequate organ perfusion, general malaise, chest pain, syncope, shortness of breath, hemodynamic collapse, and potentially sudden cardiac arrest or death.
Illustrated Flow:
- Loss of coordination between atria and ventricles → AV dissociation → Capture beat/Fusion beat.
- Symptoms: Palpitations, hypotension, Cannon A waves.
- Organs affected: Muscles, heart, brain.
Outcome:
- Inability to respond to increased cardiac demand, leading to severe complications, including death.
WPW
Pathophysiology:
- Congenital Accessory Pathway: An alternative electrical conduction pathway from the atria to the ventricles.
- Wolff-Parkinson-White Pattern: ECG findings showing isolated ventricular pre-excitation.
- Wolff-Parkinson-White Syndrome: ECG findings associated with supraventricular arrhythmias.
Mechanism:
- Impulse travels faster along the accessory pathway, shortening the time between atrial and ventricular depolarization (Short PR interval <0.12 sec).
- Early ventricular depolarization (preexcitation) leads to wide QRS complex with a delta wave.
- Altered ventricular repolarization results in ST and T-wave changes.
Arrhythmias:
- Orthodromic AVRT: Narrow QRS complex tachycardia.
- Antidromic AVRT: Wide QRS complex tachycardia.
- Pre-excited Atrial Fibrillation: Wide, irregular QRS complex tachycardia.
Clinical Notes:
- WPW pattern is more common than WPW syndrome.
- Patients may also experience atrial flutter, AVNRT, ventricular tachycardia, and ventricular fibrillation.
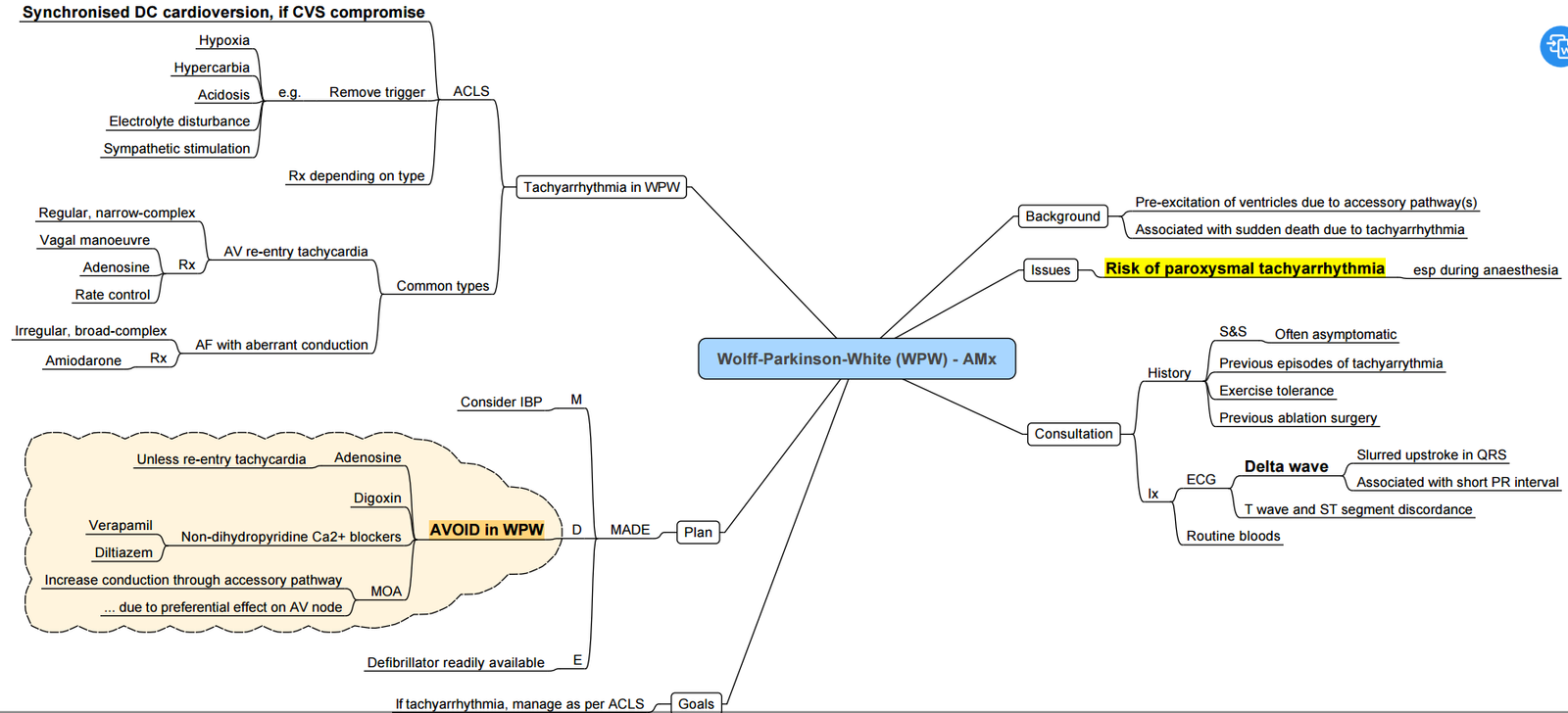
Management of Wolff-Parkinson-White Syndrome
Acute Management
- Unstable: Synchronized DC shock.
- Stable: Anti-arrhythmic to prolong the accessory pathway refractory period:
- Sotalol
- Amiodarone
- Flecainide
- Procainamide
- Contraindicated Drugs:
- Digoxin (shortens refractory period)
- Verapamil and lignocaine (increase ventricular rate)
- Beta-blockers (no effect on accessory pathway refractory period)
Long-term Management
- Radio-frequency ablation
Atrial Flutter
Atrial Flutter: Pathogenesis and Clinical Findings
Pathophysiology:
- Causes: Rheumatic heart disease, idiopathic, LV dysfunction, iatrogenic (cardiac surgery).
- Mechanism:
- Spontaneous premature depolarization of atrial tissue
- Depolarization wave propagates around atrial free-wall myocardium.
- The “re-entry loop” electrical impulse circulates at a rate of 180-350/min, usually in the right atrium.
- Electrical Conduction:
- Tissue of the tricuspid valve annulus conducts the wave.
- Conduction of depolarization wave through atrial septum.
- AV node conducts only if not in a refractory state.
- ECG Findings:
- Saw-tooth P waves (waves inverted in leads II, III, and aVF).
- Short PR interval (<0.12 sec).
- 1 QRS complex per 2-5 atrial P waves.
- Clinical Manifestations:
- Heart Rate: Pulse of 60-200 bpm.
- Symptoms: Dyspnea, presyncope, fatigue.
- Carotid massage or vagal maneuvers decrease AV node conductivity, leading to transient decreases in ventricular rate.
- If high ventricular rate decreases diastolic filling time, cardiac output decreases, leading to ineffective perfusion of body tissues.
- Other Notes:
- WPW pattern is more common than WPW syndrome, both rare (<1%).
- Other arrhythmias can occur with WPW: atrial flutter, AVNRT, ventricular tachycardia, and ventricular fibrillation.
- ST and T wave changes present in the opposite direction to the QRS complex and delta wave.
Torsade’s Des Points
Pathophysiology
- Causes:
- Acquired Long QT Syndrome: Drugs (Class 1A, Class III, TCAs, erythromycin), sinus bradycardia, AV block, metabolic abnormalities (hypo K+/Ca2+/Mg2+), primary heart disease (ischemic, congestive heart failure, cardiomyopathy).
- Congenital Long QT Syndrome: Mutated cardiac ion channels, leading to decreased repolarizing current/increased depolarizing current in cardiomyocytes.
- Mechanism: Prolonged ventricular action potential duration → Early after depolarization (EAD) → Triggering PVC → Functional re-entry.
ECG Findings
- QTc Interval: Prolonged.
- ECG Changes: Polymorphic ventricular tachycardia with shifting QRS morphology.
Clinical Manifestations
- Non-sustained TdP: Asymptomatic, palpitations, syncope.
- Sustained TdP: Degeneration to ventricular fibrillation (VF), sudden cardiac death.
Management
Unstable:
Defibrillation (200J biphasic)- may not be able to lock onto a QRS complex so may need to be unsynchronised.
Stable:
IV magnesium 2g over 15 mins, followed by 1g per hour.
Treat any hypokalaemia.
Stop all medications that prolong QT.
If refractory:
Speed up the heart:
Chemically: adrenaline infusion, dobutamine or isoproterenol.
Electrically: transcutaneous pacing.
Lignocaine 1-1.5mg/kg
Ventricular Fibrillation
Pathophysiology
- Channelopathies: Alterations in ion transport (e.g., Long QT or Brugada Syndromes).
- Accessory Pathway: Alternatives for impulse conduction.
- Structural Abnormalities: Congenital or acquired heart defects (e.g., cardiomyopathy, MI, cardiac surgery, ARVD).
Trigger Events
- Acute myocardial infarction (AMI)
- Dysrhythmias
- Electrolyte abnormalities (K+, Mg2+, Ca2+)
- Hypoperfusion
- Hypothermia
- Hypoglycemia
- Trauma
- Drugs
Mechanism
- An acute trigger event can precipitate ectopic electrical activity and multiple micro-re-entry circuits.
- Disorganized electrical activity interferes with normal conduction, causing uncoordinated ventricular contraction.
Clinical Findings
- ECG: Disorganized without identifiable QRS or T waves.
- Symptoms: Loss of consciousness, no palpable pulse, no heart rate (HR), no blood pressure (BP).
- Complications: Clinical cardiac arrest, global hypoperfusion, multi-system organ failure, hypoxic brain, brain damage, brain death, death.
Note: Ventricular fibrillation is a medical emergency requiring CPR and defibrillation.
Links
- Anti-arrhythmic drugs
- Atrial fibrillation
- Anaesthesia emergencies
- Electrocardiogram (ECG)
- Advanced cardiac life support (ACLS)
References:
- Hutchins, D. (2013). Peri-Operative Cardiac Arrhythmias: Part Two Ventricular Dysrhythmias. Anaesthesia Tutorial of the Week 285. World Federation of Societies of Anaesthesiologists. Retrieved from WFSA Resources.
- The Calgary Guide to Understanding Disease. (2024). Retrieved June 5, 2024, from https://calgaryguide.ucalgary.ca/
- FRCA Mind Maps. (2024). Retrieved June 5, 2024, from https://www.frcamindmaps.org/
- Anesthesia Considerations. (2024). Retrieved June 5, 2024, from https://www.anesthesiaconsiderations.com/
Summaries:
Copyright
© 2025 Francois Uys. All Rights Reserved.
id: “07cb2033-661f-449f-aa69-722bdbfd39ff”



