{}
Aortic Cross-Clamping
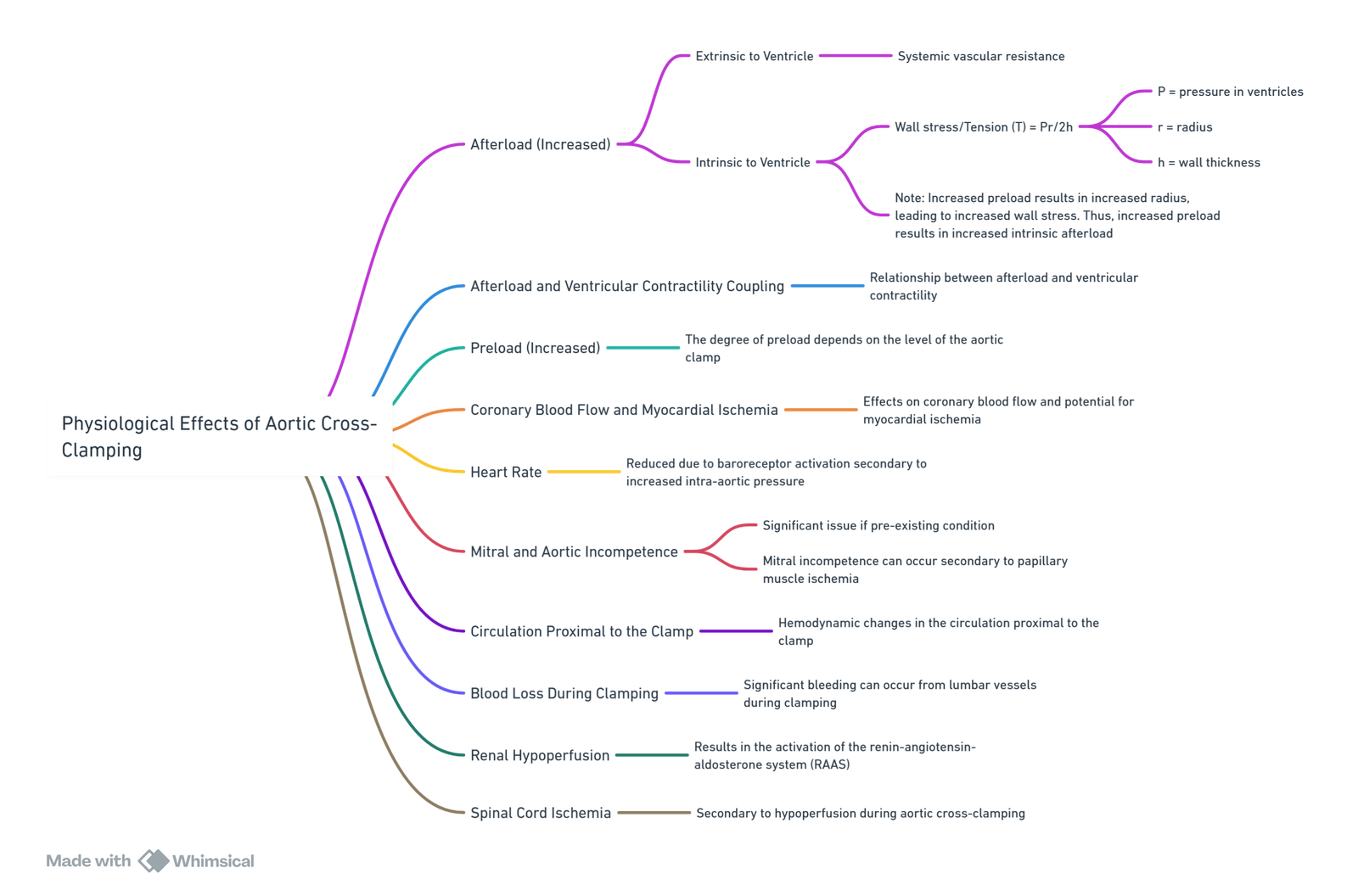
Afterload
- Afterload: The force opposing the shortening of myocardial fibers.
- Components:
- Traditionally considered external forces.
- Includes intrinsic myocardial forces that oppose fiber shortening.
Extrinsic Afterload
- Three-Element Windkessel Model:
- Components: Impedance, aortic compliance, peripheral vascular resistance.
- Effective Arterial Elastance (Ea): A simple afterload descriptor, calculated as the ratio of end-systolic pressure (mean arterial pressure) to stroke volume. An increase in the Ea slope indicates an increase in afterload.
Intrinsic Afterload
- Wall Stress-Tension:
- Influenced by ventricular pressure (P), radius (r), and wall thickness (h).
- Determinants:
- Wall stress affects myocardial oxygen supply and demand. Increased wall stress increases demand and reduces supply, potentially causing ischemia.
- Ventricular radius impacts wall tension, where increased preload increases afterload and affects oxygen supply-demand balance.
Ventricular-Load Coupling
- Coupling Dynamics:
- Parabolic relationship between left ventricular stroke work and afterload.
- Stroke work increases with increased stroke volume and arterial pressure.
- The descending limb indicates ventricular failure as stroke volume decreases with increasing afterload.
- Contractility shifts the curve: higher contractility improves tolerance to afterload.
Key Factors
-
Increase in Left Ventricular Afterload:
- Influenced by:
- Clamp Level: Higher clamps increase afterload more significantly.
- Thoracic Aorta Clamping:
- Increases mean arterial and pulmonary pressures, decreases cardiac index.
- Supracoeliac Clamping:
- Increases mean arterial pressure, decreases ejection fraction, and causes myocardial ischemia.
- Infrarenal Clamping
- Minimal changes, no wall motion abnormalities.
- Thoracic Aorta Clamping:
- Aortic Disease: Aortic occlusive disease shows less afterload increase due to collateralization.
- Clamp Level: Higher clamps increase afterload more significantly.
- Influenced by:
-
Left Ventricular Function:
- Normal ventricles handle afterload increases better but can fail with significant afterload.
- Anrep Effect: Increased contractility following afterload increase, possibly due to increased coronary blood flow and autoregulation recovery.
-
Coronary Artery Disease and Myocardial Ischemia:
- Increases in preload and afterload raise oxygen demand and limit supply.
- Duration of Clamping: Longer durations worsen vascular resistance and reduce cardiac output.
-
Preload Increases:
- Seen with higher clamps, resulting in increased left ventricular end-diastolic volumes and pressures.
- Mechanisms:
- Blood Volume Redistribution: Arterial recoil and venoconstriction.
- Afterload-Induced Preload: Ventricular dilation to maintain stroke volume.
-
Wall Tension:
- Increased ventricular radius raises wall tension and myocardial ischemia risk.
Management of Aortic Cross Clamping
- Manage left ventricular contractility, afterload, preload, ventricular dilation, myocardial ischemia, and clamp height.
Myocardial Preservation
- Goals: Decrease afterload, normalize preload, improve coronary blood flow and contractility.
- Methods: Bypass/shunt during thoracic clamping, vasodilators during lower clamping.
Specific Medications
Nitroglycerine
- Uses: Prevent/manage myocardial ischemia.
- Mechanism: Venodilator (low dose), arteriolar dilator (high dose).
- Advantages: Does not increase heart rate at low dosages.
Magnesium
- Advantages: Calcium channel blocker, alpha-1 blocker, arteriolar dilator, improves diastolic function, anti-arrhythmic, analgesic.
Volatile Anesthetic Agents
- Isoflurane: Significant vasodilation, not advisable as the sole vasodilator.
- Sevoflurane and Halothane: Increase myocardial blood flow, reduce platelet adhesion, induce pharmacological preconditioning.
Inotropic Support
- Essential during clamping, especially with inodilators, to manage hemodynamic effects.
Thoracic Epidural
- Reduces sympathetic outflow, increases venous capacitance, improves myocardial oxygen supply-demand balance.
Summary of Management
- Anaesthesia Depth: Maintain with inhalation agents and thoracic epidural.
- Fluid Management: Avoid increases in wall tension.
- Heart Rate Control: Titrate beta-blockers.
- Venous Return Manipulation: Patient positioning.
- Vasodilators: Use for circulation and coronary supply-demand balance.
- Inotropic Support: Continue during clamping.
Unclamping
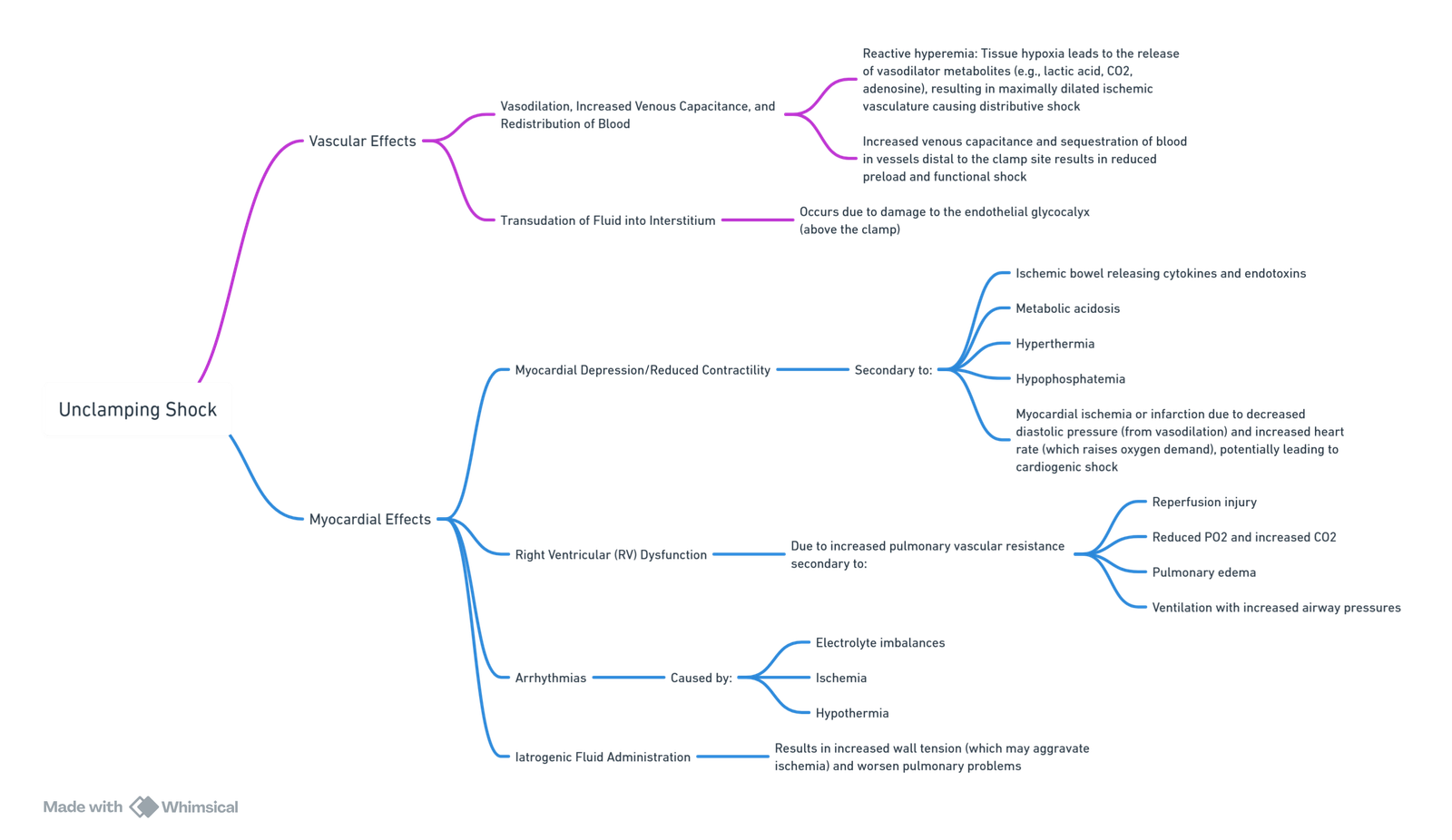
Declamping Shock
- Cardiac Output: Increases in response to decreased afterload.
- Arterial Blood Pressure and Systemic Vascular Resistance: Reductions due to vasodilation and exposure to vasoactive substances.
- Myocardial Depression: Caused by cytokines and endotoxins from ischemic bowel.
Effects Above and Below the Clamp
- Proximal: Vasodilation, increased venous capacitance, myocardial ischemia risk.
- Distal: Reactive hyperemia, reduced venous return.
Other Contributing Factors
- Oxygen Radical Formation: Reperfusion injury.
- Inflammatory Response: Various mediators.
- Lung and Reperfusion: Pulmonary hypertension, increased alveolar ventilation, potential alveolar edema.
- Kidney: Renin-angiotensin system activation, importance of renal perfusion, hyperkalemia risk.
Management of Unclamping
- Preparation: Start 10 minutes before unclamping.
- Fluids: Administer colloids to increase PAWP/CVP.
- Vasopressors/Inotropes: Support blood pressure and cardiac function.
- Nitroglycerine: Low-dose to manage wall tension.
- Leg Elevation: Augment venous return.
- Maintain Mean Arterial Pressure: Use vasopressors to ensure adequate perfusion.
Summary of Unclamping Hypotension Causes
- Hypovolemia from blood pooling.
- Ischemia-mediated vasodilation.
- Accumulation of vasoactive/metabolites.
Links
- Endovascular Abdominal Aortic Aneurysm Repair (EVAR)
- Cardiac surgery
- Aortic surgery
- Thoracic emergencies
References:
- Levin, A. (2010). The cardiovascular effects of aortic clamping and unclamping. Southern African Journal of Anaesthesia and Analgesia, 16(2), 62–71.(https://www.tandfonline.com/doi/full/10.1080/22201173.2010.10872666)
Summaries:
Copyright
© 2025 Francois Uys. All Rights Reserved.
id: “70c1d4ac-7faa-445c-94a8-ca0e6d7424fb”



