{}
Conduct of Anaesthesia
Summary
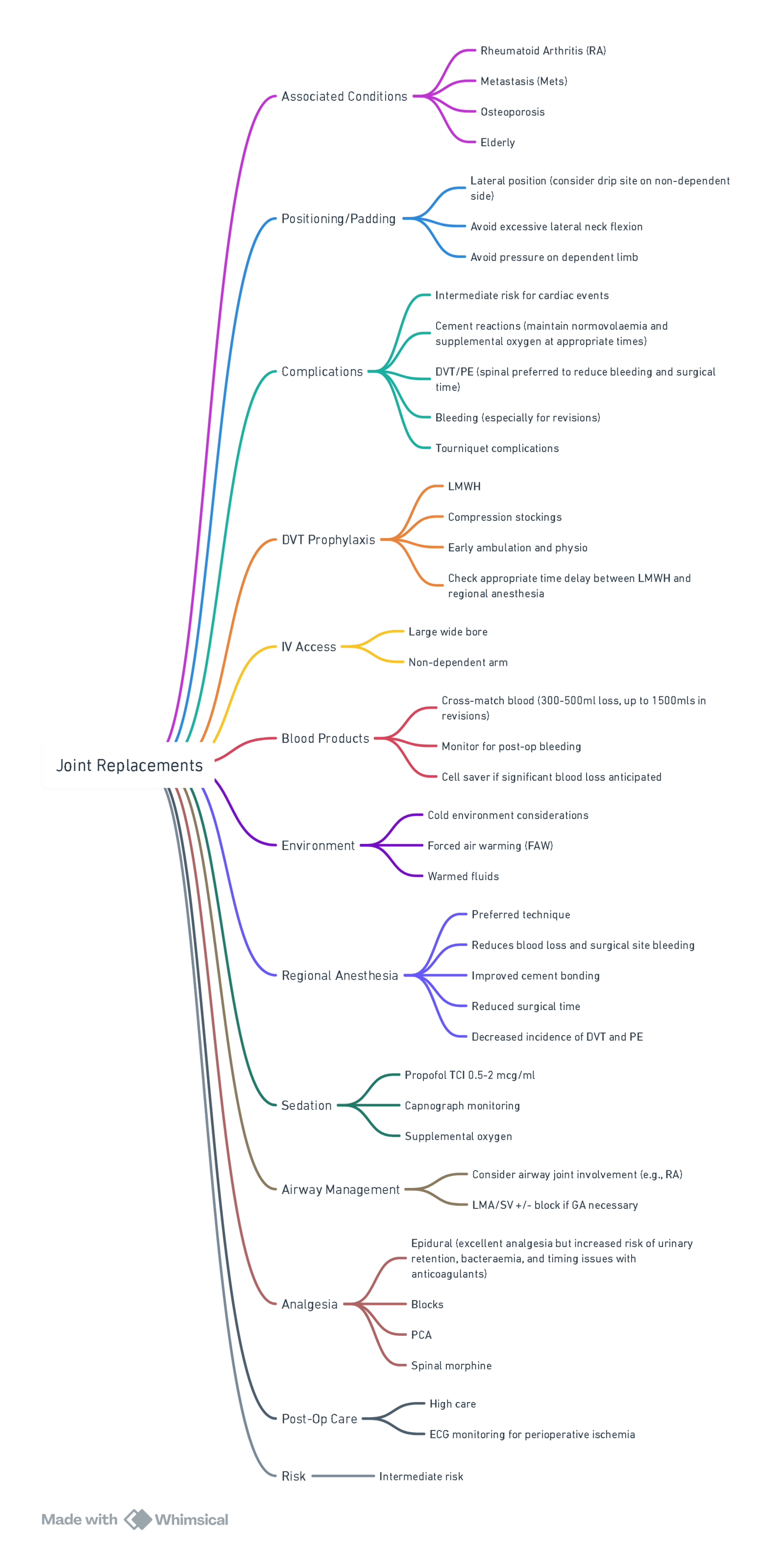
View or edit this diagram in Whimsical.
Joint Replacement–Conduct of Anaesthesia
Pre-operative Assessment & Optimisation
- Comorbidity & Frailty–document ASA status, frailty score, pulmonary hypertension, obstructive sleep apnoea (OSA) and renal function.
- Anaemia & Nutrition–screen ≥ 4 weeks pre-op; treat iron-deficiency (i.v. ferric carboxymaltose 15 mg kg⁻¹), optimise diabetes (HbA1c ≤ 64 mmol mol⁻¹) and albumin.
- Thrombosis Prophylaxis Plan–stratify venous thrombo-embolism (VTE) risk; commence mechanical measures on admission and prescribe chemical prophylaxis for day 0.
- Patient Education & Expectations–counsel on early mobilisation and realistic pain trajectories; provide written ERAS information.
- Lifestyle Optimisation–smoking and alcohol cessation ≥ 4 weeks; personalised exercise (“pre-habilitation”).
Persistent Post-Surgical Pain (PPSP)–Risk Factors
| Domain | High-risk Features |
|---|---|
| Psychosocial | Pain catastrophising, anxiety, depression, poor coping style |
| Pre-existing pain | Severe chronic joint pain, neuropathic descriptors, multisite pain |
| Biological | Younger age (< 60 yr), high BMI, dyslipidaemia, sleep disturbance, central sensitisation |
| Medication | Long-term opioids, gabapentinoids, high pre-op analgesic burden |
- Pre-operative identification permits targeted education, pre-emptive multimodal analgesia and early chronic pain follow-up.
Anaesthetic Technique
Neuraxial versus General Anaesthesia
| Setting | Best current evidence | Signal for NA benefit |
|---|---|---|
| Urgent hip-fracture surgery | REGAIN (pragmatic RCT, 1 600 pts) | No reduction in mortality or major morbidity; functional recovery equal. |
| Elective THA/TKA | 2024 US-national database (>2 million cases) & other registries | Reduced transfusion, pulmonary complications, AKI and 30-day mortality with NA, even after propensity matching. |
| Meta-analyses 2024–25 (mixed urgency) | Heterogeneous; pooled estimates favour NA for pulmonary complications and transfusion but not for mortality when only high-quality RCTs included |
- Elective total joint arthroplasty: Large observational datasets continue to show lower transfusion requirements, pulmonary complications, acute kidney injury and small absolute reductions in 30-day mortality with NA versus contemporary GA, without delaying mobilisation.
- Hip-fracture surgery The REGAIN RCT demonstrated clinical equivalence between spinal anaesthesia (with light sedation) and protocolised GA for 60-day mortality and ambulation, suggesting that previously observed mortality benefits may be smaller or procedure-specific.
- Likely to benefit most from NA: patients with severe pulmonary disease, obstructive sleep apnoea, right-ventricular dysfunction or high persistent-pain risk—but evidence for mortality benefit in very elderly hip-fracture patients is now uncertain.
Regional Blocks & Local Infiltration
| Operation | Preferred Block(s) | Remarks |
|---|---|---|
| THA | Pericapsular nerve group (PENG) ± fascia iliaca | Preserves motor power; facilitates early mobilisation |
| TKA | Adductor canal ± iPACK (infiltration between popliteal artery & capsule of the knee) | Provides sensory analgesia while sparing quadriceps; superior to femoral nerve block for mobilisation |
| Both | Local infiltration analgesia (ropivacaine 2 mg ml⁻¹ 100 ml + ketorolac 30 mg) | Evidence strong for TKA, limited for THA |
- Continuous catheter techniques are reserved for revision surgery or opioid-tolerant patients.
Intra-operative Management
- Monitoring–arterial line for ASA ≥ III, goal-directed fluid therapy (stroke-volume variation or oesophageal Doppler).
- Antibiotic Prophylaxis–cefazolin 2 g i.v. within 60 min of incision (add vancomycin 15 mg kg⁻¹ if MRSA risk).
- Antifibrinolytic–TXA 15 mg kg⁻¹ i.v. at induction ± repeat 3 h later; single dose is non-inferior to multiple doses for primary arthroplasty. Oral TXA 2 g pre-incision is an effective alternative.
- Temperature Management–forced-air or under-body conductive warming; target core 36 °C.
- Fluid & Blood Loss
- Use an individualised, goal-directed fluid strategy that maintains euvolaemia and avoids both fluid overload and cumulative deficit._ In uncomplicated primary arthroplasty this usually equates to a near-zero to modestly positive (< +0.5 L) balance by skin closure, switching to oral fluids in recovery.
- Consider advanced haemodynamic monitoring (SVV/PPV, oesophageal Doppler) in ASA ≥ III, revision or bilateral cases.
- Transfuse at Hb < 80 g l⁻¹ (or < 90 g l⁻¹ if symptomatic coronary disease).
- Tourniquet–lowest effective pressure; deflate before closure to allow haemostasis.
- Bone Cement–apply BCIS precautions (see dedicated note).
Fluid Management in Contemporary Hip & Knee Arthroplasty — where Are We Now?
| What has changed? | Why? | Practical takeaway for elective TJA |
|---|---|---|
| Strict zero-balance (≤ 1 L positive at end of case) no longer recommended for major procedures | ▸ RELIEF RCT: restrictive strategy ↑ acute kidney injury 8.6 % vs 5 % liberal Surgery”▸ Subsequent meta-analyses show U-shaped harm curve (both deficit and overload) | Aim euvolaemia rather than absolute zero |
| Consensus groups now advise a moderately positive balance for moderate–major surgery | 2024 POQI XI consensus: target +1–2 L for major cases; ~+0.5–1 L for shorter procedures | For primary THA/TKA (blood loss usually < 500 mL) a near-zero to modest positive balance is still appropriate. |
| ERAS TJA guideline reframes the question: “Maintain fluid balance, avoid both overand under-hydration.” | ERAS Society hip/knee statement stresses judicious IV fluids & early oral intake, not fixed volumes | Stop IVF as soon as the patient tolerates oral intake; replace measured losses only. |
| Goal-directed haemodynamic therapy (GDFT) favoured for high-risk or revision surgery | Small orthopaedic studies & larger meta-analyses show fewer hypotensive minutes and shorter stay with SV-guided GDFT | Use oesophageal Doppler/arterial pressure waveform in ASA ≥ III or revision arthroplasty; give bolus only if fluid-responsive and hypoperfused. |
Post-operative Care
Multimodal Analgesia
- Scheduled–paracetamol 1 g 6-hourly; NSAID or COX-2 inhibitor if no contra-indication.
- Regional–continuation of catheter technique where used; consider single-shot adductor canal block top-up at 12 h for TKA.
- Systemic Rescue–i.v. morphine PCA (1 mg bolus, 5 min lock-out) titrated for Was < 4; low-dose ketamine infusion (0.1 mg kg⁻¹ h⁻¹) in opioid-tolerant patients.
- Adjuncts–dexamethasone 4 mg, ondansetron 4 mg for PONV prophylaxis; gabapentinoids not recommended routinely.
Thromboprophylaxis & Early Mobilisation
- Mechanical prophylaxis on day 0; chemical prophylaxis (LMWH 40 mg s.c. daily or DOAC per protocol) from 6 h post-surgery.
- Physiotherapy to standing on day 0 and ≥ 30 m ambulation day 1.
Neuraxial Anaesthesia & Anticoagulation (ASRA 2025)
| Agent | Minimum delay before block | Catheter removal | Restart after removal |
|---|---|---|---|
| LMWH prophylaxis (40 mg od) | 12 h | ≥ 12 h after last dose | ≥ 6 h |
| LMWH treatment (1 mg kg⁻¹ bid) | 24 h | Contra-indicated | – |
| UFH s.c. (< 15 000 units day⁻¹) | 4 h | 4–6 h | 1 h |
| Apixaban / Rivaroxaban | 72 h (check anti-Xa if < 72 h) | Contra-indicated | ≥ 6 h |
| Dabigatran (CrCl ≥ 50 ml min⁻¹) | 72 h | Contra-indicated | ≥ 6 h |
| NSAIDs, aspirin ≤ 325 mg day⁻¹ | No restriction | – | – |
| Thrombolytics | Absolute contra-indication | – | – |
Always individualise based on bleeding risk, renal function and concurrent antiplatelets.
Enhanced Recovery After Surgery (ERAS) for TJA
Core Elements
| Phase | Key Components |
|---|---|
| Pre-op | Education, carbohydrate drink (unless insulin-dependent diabetes), active pre-warming, pre-emptive oral analgesia |
| Intra-op | Spinal anaesthesia with low-dose intrathecal local anaesthetic (no opioid), TXA, normothermia, antibiotic & anti-emetic prophylaxis |
| Post-op | Opioid-sparing multimodal analgesia, early oral intake (≤ 6 h), VTE prophylaxis, day-of-surgery mobilisation, criteria-led discharge |
ERAS pathways halve median length of stay (6 → 3 days) without increasing readmission or complication rates, and confer the greatest benefit in patients ≥ 85 years. Regular audit sustains compliance and outcomes.
Evidence Summary
- NA remains the reference standard for elective TJA when feasible.
- Adductor canal ± iPACK block provides superior mobilisation compared with femoral nerve block for TKA.
- Single-dose i.v. (or 2 g oral) TXA is adequate for most primary arthroplasties.
- Multimodal, opioid-sparing regimens and early physiotherapy are central to reducing PPSP incidence.
Links
- Enhanced recovery after surgery (ERAS)
- Cement
- Tourniquets
- Ortho regionals
- Anticoagulation and blocks
References:
- Enhanced recovery after surgery in arthroplasty, N Biyase; Southern African Journal of Anaesthesia and Analgesia. 2021;27(6 Suppl 1):S214-217. https://doi.org/10.36303/SAJAA.2021.27.6.S1.2711
- Soffin, E. M. and YaDeau, J. T. (2016). Enhanced recovery after surgery for primary hip and knee arthroplasty: a review of the evidence. British Journal of Anaesthesia, 117, iii62-iii72. https://doi.org/10.1093/bja/aew362
- Shiu, Y. and Lawmin, J. (2015). Anaesthesia for joint replacement surgery. Anaesthesia &Amp; Intensive Care Medicine, 16(3), 89-92. https://doi.org/10.1016/j.mpaic.2014.12.009
- ERAS® Society. Consensus statement for perioperative care in total hip and knee replacement surgery. Acta Orthop 2019. PMC
- Enhanced recovery after surgery protocols for total joint arthroplasty–current evidence. Perioper Med 2023. PMC
- Comparative effectiveness of neuraxial versus general anaesthesia in contemporary THA/TKA patients. Anesthesiology 2024. PubMed
- Is outcome improved with neuraxial anaesthesia in total joint arthroplasty? J Arthroplasty 2024. arthroplastyjournal.org
- Impact of neuraxial anaesthesia on postoperative acute kidney injury. Curr Opin Anaesthesiol 2025. SpringerLink
- Adductor canal block versus femoral nerve block: network meta-analysis. Anaesthesia 2024. PubMed
- Review: adductor canal block in TKA. Int Orthop 2025. ScienceDirect
- Systematic review–factors associated with PPSP after TKA/THA. Pain 2023. [PMC](https://pmc.ncbi.nlm.nih.gov/articles/PMC9833456/?utm_source=chatgpt.com
- Risk factors for chronic postoperative pain after TKA: meta-analysis. J Orthop Surg Res 2024. BioMed Central
- Long-term pain prevalence after TKA/THA: umbrella review. Bone Joint J 2025. PMC
- AAOS/AHKS endorsed clinical guidelines: TXA in total joint arthroplasty. AAOS 2018 (still current). American Academy of Orthopaedic Surgeons
- Randomised study–multiple versus single i.v. TXA doses in TKA. J Clin Orthop Trauma 2025. Journal of Orthopaedic Case Reports
- American Society of Regional Anaesthesia (ASRA) Evidence-Based Guidelines: anticoagulation & regional anaesthesia, 5th Edition 2025. rapm.bmj.comGuideline Central
Summaries:
Regionals for hip fractures
Lower limb blocks
Analgesia for hips and knees
Copyright
© 2025 Francois Uys. All Rights Reserved.
id: “d4e00eed-9b11-43d9-92d7-391186057c01”



