- Advantages of Regional Anaesthesia versus General Anaesthesia
- Upper Limb
- Elbow Blocks
- Comparison Between the ASRA Regional Anesthesia and Pain Guidelines
- Procedural Anticoagulation Management Checklist
- 1. Evaluate Baseline Patient-Specific Risk Factors for Perioperative Bleeding
- 2. For Individuals on Aspirin Categorize Reason for Utilization
- 3. Process the Anatomical Location of Procedural Intervention into Decision-Making
- 4. Review Appropriate Radiographic Imaging to Identify and Understand Anatomic Challenges
- 5. Identify and Manage Pharmacologic Coagulopathies
- 6. Employ Post-Procedure Surveillance for the Detection of Bleeding Complications
- Stratification of Risk According to Procedures
- Recommendations for Thromboprophylaxis in Nonorthopedic Surgical Patients
- Warfarin
{}
Advantages of Regional Anaesthesia versus General Anaesthesia
- Reduction of nausea and vomiting
- A decreased stress response
- Excellent quality of analgesia both perioperatively and postoperatively, avoiding the systemic side effects associated with other analgesics
- Possible pre-emptive analgesia and, theoretically, a reduction in sensitization of nerve endings after surgery with a reduction in chronic pain syndromes
- Earlier patient discharge owing to improved analgesia and earlier mobilization
- Reduction of blood loss because of relative hypotension with central neural blockade
- Economic benefit to the hospital, as drug and equipment costs are consistently lower for regional anaesthesia and patients have shorter in-hospital stay
- Enhanced communication and easier positioning of the patient, who will be conscious throughout the surgery
- Avoidance of airway instrumentation and cervical movement during the operation, which is particularly important for patients with rheumatoid arthritis and ankylosing spondylitis
- Reduced environmental exposure to anaesthetic gases
Why Ultrasound
- For adequately imaged nerves, a positive motor response to nerve stimulation does not improve the success of the block. A block could be successful without positive nerve stimulation. Muscle stimulation and paraesthesia may not occur even when ultrasound confirms the correct needle position. The needle can be intraneural and there can still be failure to provoke muscle contractions by the nerve stimulator.
- In diabetic patients, nerve stimulation and paraesthesia may be impossible to elicit at currents below 2 mA. Contrary to conventional belief, nerve puncture and intraneural injection of LA does not always lead to nerve injury.
Contra-indications to Regional Anaesthesia
- Patient’s refusal despite adequate explanation
- Confused, uncooperative or uncommunicative patient
- Systemic infection, trauma/burns/local infection over the site of injection
- Pre-existing neurological deficit (relative)
- Raised intracranial pressure (central neural blocks)
- Untreated hypovolaemia, hypotension or heart failure (central neural blocks)
- Anticoagulated/coagulopathic patient
Upper Limb
Upper Limb Blocks
- The upper extremity is well suited to peripheral nerve blockade because the entire arm and shoulder are innervated by the brachial plexus and blockade is easily accomplished with a single injection.
- The selection of regional technique will be dependent on the anticipated site of surgery as well as the site of the tourniquet. The interscalene approach is well suited for proximal surgery on the shoulder joint and upper arm; the supraclavicular approach is preferable for the upper arm, elbow, and radial side of the forearm and can provide a dense block of the arm providing optimal tourniquet coverage as well; the infraclavicular and axillary approaches are best for the hand, wrist, and forearm.
Dermatomes
- Occipital: C2
- Supraclavicular: C3-C5
- Suprascapular: C5-C6
- Subclavius: C5-C6
- Long thoracic: C5-C7
- Subscapular: C5-C6
- Axillary: C5-C6
- Intercostal: T3-T12
- Primary nerve branches
- Intercostobrachial: T2
- Cutaneous brachii medialis: C8-T1
- Musculocutaneous: C5-C6
- Median: C5-T1
- Ulnar: C8-T1
- Radial: C5-T1
- Cutaneous antebrachii medialis: C8-T1
Innervation
- Five major terminal nerves come from the plexus (axillary, musculocutaneous, median, ulnar, and radial) and these can be blocked individually or in combination to provide analgesia.
- A major advance is the placement of indwelling brachial plexus catheters to provide prolonged analgesia at home, thereby allowing operations that would have traditionally required 2-3 days of hospitalization to be performed as day-stay or short-stay surgery.
Brachial Plexus
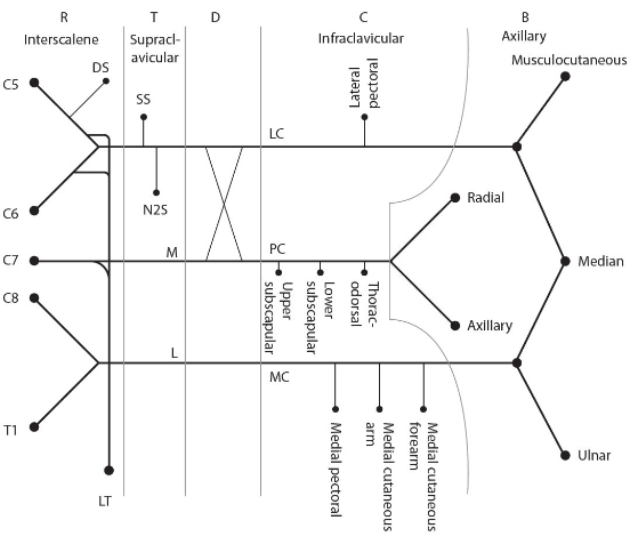
The brachial plexus is formed by the anterior primary rami of the lower four cervical nerve roots (C5-C8) and the first thoracic nerve root (T1). It supplies sensory and motor innervation to the entire upper limb except for the trapezius muscle (innervated by the spinal accessory nerve) and the cutaneous innervation of the axilla (supplied by the intercostobrachial nerve).
Structure of the Brachial Plexus
Roots
- The ventral rami of C5-T1 spinal nerves form the five roots of the plexus.
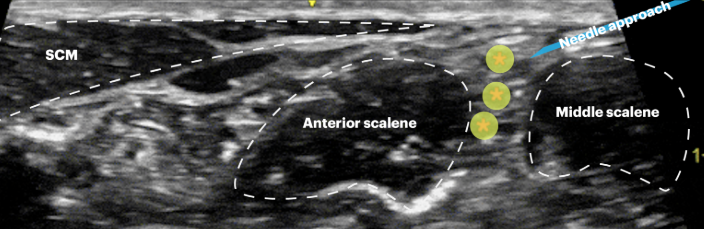
- An interscalene block mainly targets the upper roots (C5-C7). Due to the vertical arrangement of the brachial plexus roots in the interscalene groove, C8 and T1 are often missed, hence the ulnar nerve may not be blocked.
Trunks
- Shortly after leaving the intervertebral foramina, the roots unify to form three trunks:
- Upper (C5-C6)
- Middle (C7)
- Lower (C8-T1)
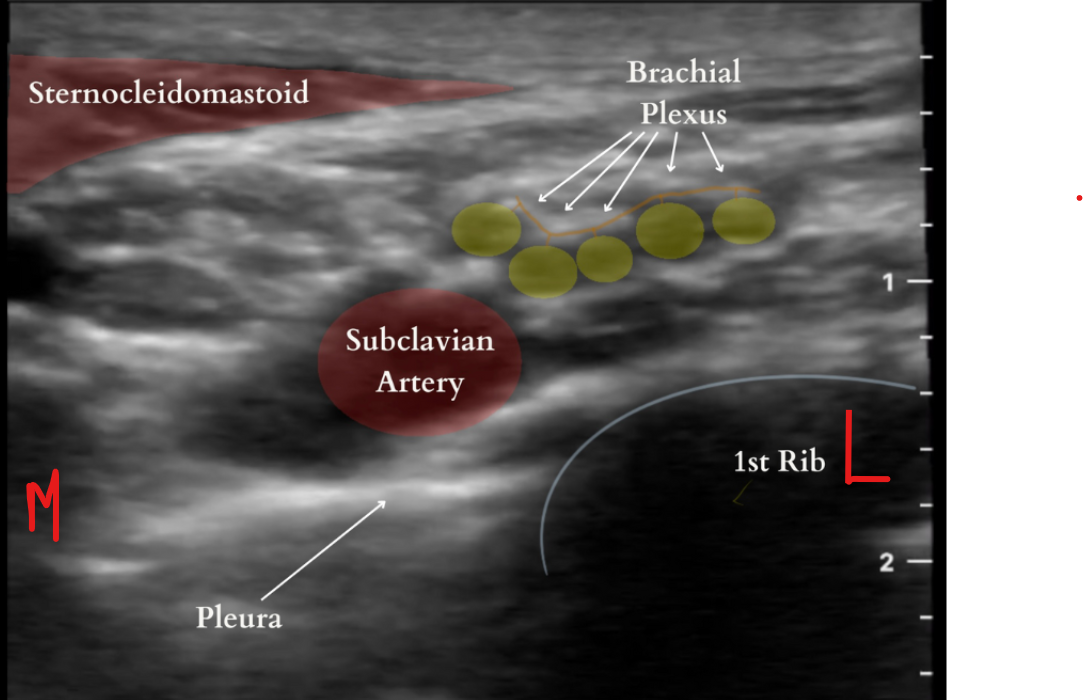
- Supraclavicular blocks are performed at the level of the brachial plexus trunks to more reliably block the entire upper limb.
Divisions
- Each trunk divides into two divisions, forming six divisions in total (three anterior and three posterior).
- The divisions generally cannot be blocked reliably because they lie behind the clavicle.
Cords
- The six divisions unite again to form three cords:
- Posterior cord (C5-T1) formed by the posterior divisions.
- Lateral cord (C5-C7) formed by the anterior divisions from the upper and middle trunks.
- Medial cord (C8-T1) formed by the anterior division of the lower trunk.
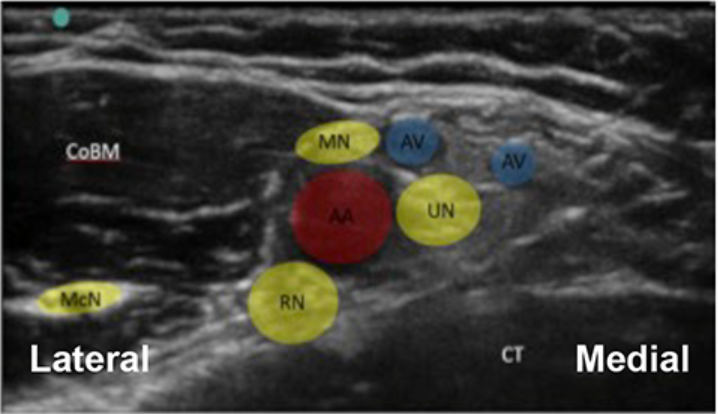
- The brachial plexus cords are named according to their relation to the axillary artery.
- Infraclavicular blocks are performed at the level of the cords and can achieve anaesthesia of the entire arm.
Terminal Branches
- Mixed nerves containing sensory and motor nerve fibres.
- Ulnar nerve (C8, T1): Arises from the medial cord. Provides motor innervation to the intrinsic muscles of the hand and sensation to the medial one and a half fingers.
- Musculocutaneous nerve (C5, C6, C7): Derived from the lateral cord. Provides motor innervation to the flexor muscles (coracobrachialis, biceps brachii, brachialis) and sensory innervation to the lateral surface of the forearm. Continues as the lateral cutaneous nerve of the forearm.
- Median nerve (C5-T1): Arises from both the medial and lateral cords. Provides motor innervation to most flexor muscles in the forearm and thenar muscles of the thumb. Provides cutaneous innervation to the thumb, index finger, middle finger, lateral half of the ring finger, and nail beds of these fingers.
- Radial nerve (C5-T1): The largest branch of the brachial plexus, derived from the posterior cord. Provides motor innervation to the extensor muscles of the elbow, wrist, and fingers, and sensation to the dorsum of the hand. Continues as the posterior cutaneous nerve of the forearm.
- Axillary nerve (C5-C6): Arises from the posterior cord. Supplies the deltoid and teres minor muscles and provides sensation below the shoulder. Continues as the lateral cutaneous nerve of the arm.
- Axillary blocks are performed at the level of the terminal branches and depend on the relationship of nerves to the axillary vessels.
Supraclavicular Branches
- Derived from the brachial plexus but provide innervation above the clavicle.
- Long thoracic nerve (C5, C6, C7): Supplies the serratus anterior muscle.
- Dorsal scapular nerve (C5): Supplies the rhomboid muscles and levator scapulae muscle.
- Nerve to the subclavius (C5, C6): Supplies the subclavius muscle.
- Suprascapular nerve (C4, C5, C6): Supplies the supraspinatus and infraspinatus muscles.
Branches of the Cords of the Brachial Plexus
Posterior Cord Branches (ULTRA)
- Upper subscapular
- Lower subscapular
- Thoracodorsal
- Radial
- Axillary
Lateral Cord Branches (LLM)
- Lateral pectoral
- Lateral root of the median nerve
- Musculocutaneous
Medial Cord Branches (MMMUM)
- Medial pectoral
- Medial cutaneous nerve of the arm
- Medial cutaneous nerve of the forearm
- Ulnar
- Medial root of the median nerve
Shoulder Blocks
- A block of at least the upper two roots (C5 and C6) or the superior trunk of the brachial plexus is necessary.
- Blockade of the supraclavicular nerve is also needed, covering the ‘cape’ of the shoulder.
- The interscalene approach is best suited for shoulder joint and upper arm surgery, targeting the roots as they exit between the middle and anterior scalene muscles at the C6 level (identified by the cricoid cartilage).
- Complications can include blockade of the cervical sympathetic chain, recurrent laryngeal nerve, phrenic nerve blockade, hypotension, bradycardia, accidental epidural and spinal injection, and permanent spinal cord damage.
- Catheter placement into the brachial plexus allows continuous local anaesthetic infiltration for painful procedures like shoulder arthroplasties, facilitating earlier mobilization. However, this technique does not provide superior postoperative analgesia compared to infusion through an intra-articular catheter.
- For shoulder arthroscopy, a suprascapular nerve block can be used but should be combined with general anaesthesia for adequate analgesia.
Interscalene Block
Elbow Blocks
- Surgery on the elbow may be performed with an interscalene, supraclavicular, infraclavicular, or axillary brachial plexus block or a mid-humeral block with cutaneous infiltration of the medial cutaneous nerve of the arm.
- An axillary approach may not be adequate for mid or distal humerus surgery due to the close proximity of the level of blockade to the site of surgery and difficulty in blocking the posterior cord of the brachial plexus.
Supraclavicular Block
Hand and Forearm Blocks
- Axillary blocks are ideal for hand and forearm surgery as the four main nerves (median, ulnar, radial, musculocutaneous) can be selectively identified using ultrasound guidance and/or peripheral nerve stimulation.
- Multiple-stimulation techniques are associated with a greater success rate than single injection techniques.
- This technique is most commonly used for surgery below the shoulder, providing effective analgesia for tourniquets applied to the upper arm. Peripheral nerve blocks at the elbow, wrist, and hand may be performed individually or in combination to provide discrete, distal nerve blockade or to supplement brachial plexus blocks.
- A short-duration brachial plexus block combined with a long-lasting peripheral nerve block allows early mobilization and limb protection while maintaining good peripheral analgesia.
Axillary Block
Bier’s Block (IVRA)
Preparation
- Standard preoperative fasting intervals should be observed.
- Informed patient consent.
- Standard minimum monitoring (electrocardiograph, noninvasive blood pressure, and SpO2).
- Resuscitation equipment available.
- Patient on a tilting trolley with suction available.
- Double-cuffed tourniquet system available and checked.
Procedure
- Intravenous access in both limbs.
- Double-cuffed tourniquet on operative limb.
- Exsanguinate limb using elevation and digital arterial pressure.
- Inflate proximal tourniquet cuff to 250-300 mmHg and confirm.
- Slowly inject 0.5% prilocaine 40 ml or 40ml of 0.5% lidocaine
- Once anaesthesia is established, inflate the distal cuff to the same pressure.
- Deflate the proximal cuff after confirming the distal cuff is inflated.
- Surgical procedure can proceed.
- Do not deflate the tourniquet until a minimum of 30 minutes has elapsed.
- Observe patient for signs or symptoms of local anaesthetic toxicity.
Advantages
- Technical simplicity.
- Rapid onset and offset.
- Reliable if carried out correctly.
- Regional anaesthesia for short and simple distal limb procedures.
Disadvantages
- Unsuitable for major surgery.
- Tourniquet pain.
- Maximum duration of about 90 minutes.
- Bloodless field not possible.
- Potential for local anaesthetic toxicity.
- No effective postoperative analgesia.
Lower Limb Blocks
Dermatomes
| Nerve | Root(s) |
|---|---|
| Subcostal | T12 |
| Ilioinguinal | L1 |
| Iliohypogastric | T12-L1 |
| Lateral cutaneous nerve of the thigh | L2-L3 |
| Genitofemoral | L1-L2 |
| Obturator | L2-L4 |
| Femoral | L2-L4 |
| Saphenous | L2-L4 |
| Posterior cutaneous nerve of the thigh | S1-S3 |
| Sciatic | L4-S3 |
| Tibial | L4-S3 |
| Common peroneal | L4-S3 |
| Superficial peroneal | L4-S2 |
| Deep peroneal | L4-S2 |
| Sural | S1 |
Hip Surgery
- Lumbar paravertebral or lumbar plexus block: Used when spinal or epidural anaesthesia is contraindicated. It can provide complete analgesia of the lower limb when combined with a sciatic nerve block, especially useful in revision joint replacement where the surgery is likely to be prolonged.
- Femoral nerve block: Provides analgesia for fracture neck of femur, total hip replacement, and femoral shaft fracture.
- Three-in-one block: Targets the lateral cutaneous nerve of the thigh, obturator nerve, and femoral nerve by injecting a large volume of local anaesthetic within the neurovascular sheath, though its effectiveness can be inconsistent.
- Fascia iliaca block: A hybrid anterior lumbar plexus approach providing faster and more consistent blockade of the lateral cutaneous nerve of the thigh and femoral nerve than the ‘three-in-one’ block.
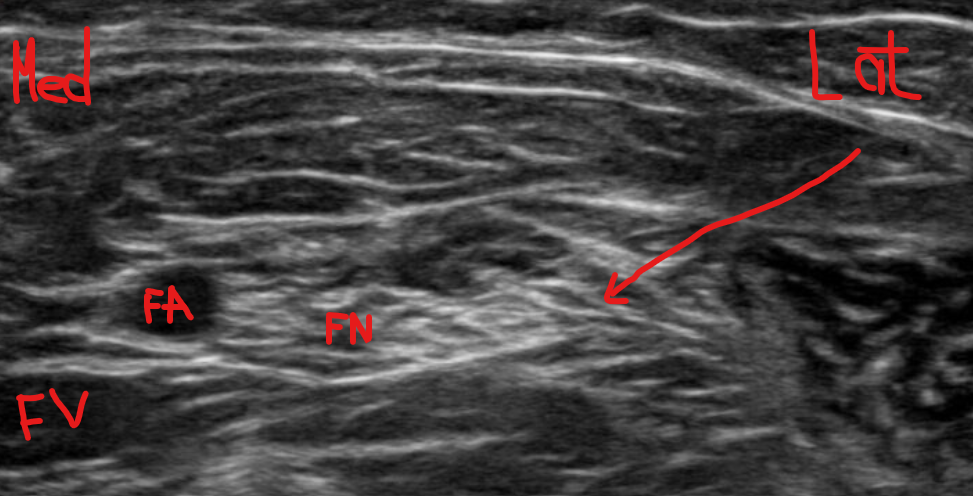
Femoral Block
Knee Surgery
- Femoral and sciatic nerve blocks: Provide intraoperative and postoperative analgesia for knee joint surgery, improve early rehabilitation by effectively controlling pain compared to intravenous morphine via patient-controlled analgesia.
- Psoas compartment block: Provides anaesthesia and analgesia to the entire lumbar plexus, used for knee arthroscopy, though not commonly justified in ambulatory patients due to risks like epidural spread and weak hip flexors.
- Femoral nerve block: Covers the anteromedial thigh, anterior knee, and medial calf, making it one of the most common lower extremity blocks.
- Intra-articular injection: A combination of ropivacaine or levobupivacaine, adrenaline, morphine, and methylprednisolone, used increasingly for total knee replacement and sometimes for total hip replacement, though further studies are needed to determine the optimal volume and concentration of the drugs. An indwelling catheter can also be used for top-ups or continuous infusion, with a risk of infection.
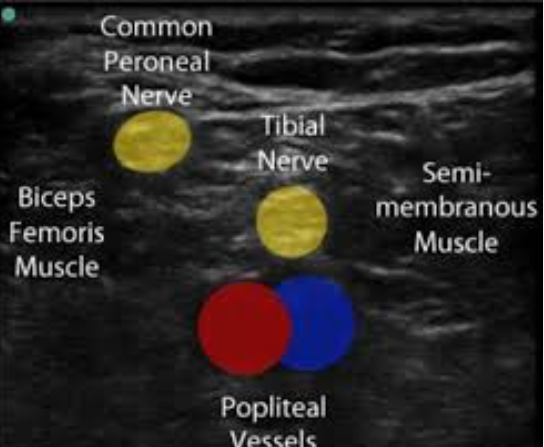
Popliteal-sciatic Block
Ankle/Foot Surgery
- Popliteal block: Effective for foot and ankle surgery, often combined with a saphenous nerve block for medial foot and ankle involvement. Adequate for a calf tourniquet in conscious patients.
- Sciatic and femoral nerve block: Used if a thigh tourniquet is required during surgery, providing good surgical anaesthesia and long-lasting postoperative pain control.
- Popliteal sciatic nerve block combined with saphenous or femoral nerve block: Allows use of a calf tourniquet and provides anaesthesia comparable with neuraxial techniques, without urinary retention and with longer postoperative analgesia (12-24 hours with long-acting local anaesthetics like ropivacaine or bupivacaine).
- Ankle block: Has minimal impact on postoperative ambulation while providing prolonged postoperative analgesia with long-acting local anaesthetics. Ideal for avoiding foot drop, hamstring, or quadriceps weakness.
Summary of All Blocks
Suggested Standard Monitoring for Nerve Blocks
Ultrasound + Nerve Stimulation + Opening Injection Pressure (OIP)
- Connect needle to nerve stimulator (0.5mA, 0.1msec, 2Hz)
- Advance needle towards the nerve or plexus
- Needle adequately placed as seen on US
- No twitch
- 1-2 mL injection of LA results in adequate spread in the desired tissue plane OIP normal <15psi
- Needle adequately placed as seen on US
- Twitch present
- Reposition the needle to assure NO twitch present at <0.5mA
- 1-2 mL injection of LA results in adequate spread in the desired tissue plane OIP normal <15psi
- Needle adequately placed as seen on US
- Complete injection
- Increase current to 1.5mA
- Adjust needle placement by US
Legend
- OIP normal (<15 psi): Based on data in both animal models and clinical trials where injection pressure required to inject local anesthetic for nerve or perineural exercise is <15 psi
Upper Limb and Trunk Peripheral Nerve Blocks
| Block | Indications | LM | Technique | Stim/end point | LA | SE/Complications | Clinical points |
|---|---|---|---|---|---|---|---|
| Superficial cervical plexus | CEA, thyroid, neck line, shoulder surgery | Midpoint of SCM | Needle along posterior border of SCM cephalad & caudal | Form ‘sausage’ along posterior border of SCM | 10 ml 0.25% Levobupivicaine | Haematoma | |
| Deep cervical plexus block | CEA, cysts, LN Bx, superficial neck surgery | Thyroid cartilage (C4), posterior border SCM, interscalene groove | Identify posterior SCM at level C4, move finer laterally to feel interscalene groove | 10-20 mm in direction of contralateral elbow until paraesthesia or C4 transverse process felt | 10 ml 0.25% Levobupivicaine | Phrenic nerve palsy, RLN palsy, stellate ganglion block, haematoma | Single injection as effective |
| Interscalene block | Shoulder and humeral surgery | Cricoid (C6), posterior border of SCM, interscalene groove | Winnie’s: Posterior border of SCM at level of C6, place finger beneath on to ant belly of scalenus anterior & move laterally to feel interscalene groove | 10-20 mm in direction of contralateral elbow, Deltoid stimulation (shoulder surgery), elbow flexion (humeral surgery) | 10-40 ml 0.25-0.5% Levobupivicaine | Phrenic nerve palsy, RLN palsy, stellate ganglion block, haematoma, epidural/spinal, vertebral artery puncture, SCI, pneumothorax | Phrenic nerve – too anterior, dorsal scapular – too posterior |
| Subclavian perivascular block | Elbow, wrist & hand surgery | Interscalene groove, subclavian artery | Identify interscalene groove & move down until subclavian artery felt or skin flattens out over supraclavicular fossa | 1.5-4 cm caudally directed posterior to the artery | 10-40 ml 0.25-0.5% Levobupivicaine | Horner’s, RLN block, Vascular puncture, haematoma, pneumothorax | NO MEDIAL ANGULATION, Ulnar border missed in 5% |
| Subcoracoid infraclavicular block | Elbow, wrist & hand surgery | Coracoid, 2 cm inferior and 1-2 cm lateral | 3-8 cm deep perpendicular in all planes | Wrist/finger extension – accept posterior cord Pectoral/elbow twitch – don’t accept as too superficial/medial/cephalad. | 10 ml 0.25% Levobupivicaine | Vascular puncture, pneumothorax, intravascular injection | NO MEDIAL ANGULATION |
| Suprascapular nerve block | Shoulder surgery | Midpoint of scapular spine, draw a line from the angle of the scapula to this point, move 1 cm superiorly | Insert needle perpendicular to skin downwards on to bone | Abduction/elevation or paraesthesia | 10-20 ml 0.5% Levobupivicaine | Pneumothorax | |
| Axillary block | Elbow, wrist & hand surgery | Axillary artery, insertion of pectoralis major | Draw a line from anterior axillary fold (pec major insertion) crossing the artery; fix artery between index & middle finger. 45° to skin proximally | Above artery: Median – index/middle finger flexion Musculocutaneous – elbow flexion, Below artery: Ulnar – thumb adduction, little finger flexion Below/behind artery: Radial – thumb extension | 7-10 ml for each nerve of 0.25-0.5% levobupivicaine | Nerve damage, arterial puncture, vascular injection | Single shot commonly misses radial/musculocutaneous |
| Midhumeral block | Elbow, wrist & hand surgery | Brachial artery in the bicipital groove at the level of deltoid insertion | Median: above artery Musculocutaneous: 45° above artery & lateral to humerus Ulnar: Below & medial to artery Radial: Below artery & humerus in spiral groove | As above | 7-10 ml for each nerve of 0.25-0.5% levobupivicaine | Bruising/bleeding | |
| Elbow blocks | Forearm/hand surgery, top up brachial plexus block | Elbow crease, brachial artery, biceps tendon | Median: medial to artery, 45 degrees to skin/proximal, 10-15 mm. Medial cutaneous nerve of forearm: SubQ medial border of biceps tendon Radial: Groove between biceps and brachioradialis, 1.5-2 cm proximal to crease Lateral cutaneous nerve of forearm: SubQ lateral border of biceps tendon Posterior cutaneous nerve of forearm: SubQ infiltration between lateral epicondyle and olecranon Ulnar: medial epicondyle (sulcus), 2 cm proximal, 1-3 cm deep 45 to skin cranially | Median: finger flexion Wrist extension alone inadequate, extension of thumb needed. Flexion ring finger, thumb adduction | 5 ml 0.5% Levobupivicaine 5-10 ml 0.5% Levobupivicaine 5 ml 0.5% Levobupivicaine 5 ml 0.5% Levobupivicaine 5 ml 0.5% Levobupivicaine | Cutaneous branches of the ulnar nerve supplying the forearm come off higher. THE MAJOR NERVES ONLY HAVE CUTANEOUS INNERVATION TO THE HAND AT THIS LEVEL | |
| Wrist Block | Hand surgery | Median: FCR & PL/ FCR Palmar cutaneous branch (median n): Palmar cutaneous branch (median n): SubQ proximal to flexor retinaculum, Ulnar: FCU, Dorsal cutaneous branch (ulnar): 2 cm proximal to crease 1 cm under FCU, Superficial radial nerve: SubQ from radial styloid to posterior aspect of the wrist | 3-5 cm proximal to crease, 45 degrees towards wrist between FCR & PL (or 1 cm medial to FCR if PL absent) SubQ proximal to flexor retinaculum SubQ over ulnar aspect of wrist SubQ from radial styloid to posterior aspect of the wrist | Parasthesia index finger, Parasthesia little finger | 3-5 ml 0.5% Levobupivicaine 3-5 ml 0.5% Levobupivicaine 3-5 ml 0.5% Levobupivicaine 5-8 ml 0.5% Levobupivicaine | Nerve damage, arterial puncture, vascular injection | |
| Bier’s block | Minor superficial surgery forearm, K wires, reduction of fractures | Apply double cuff, cannulate both arms, elevate and exsanguinate the arm, inflate lower cuff followed by upper cuff to 100 mmHg above SBP, deflate lower cuff and inject LA. Rotate cuffs every 10 mins | Keep cuff inflated >20 mins | 0.5% prilocaine (300 mg max) 0.5% lignocaine (250 mg max) | CI in children, obesity, hypertension, long operations | ||
| Paravertebral block | Rib fractures, thoracic surgery, breast surgery, open cholecystectomy, renal surgery | Spinous processes & transverse processes (TP of corresponding vertebrae) | Palpate spinous processes and mark 2.5 cm lateral its most cephalad aspect. Go perpendicular to contact transverse process (2-5 cm), re-angle to go above & advance 1-1.5 cm | LOR or intercostal muscle twitch | 5-15 ml 0.25-0.5% Levobupivicaine | Intravascular, intrathecal injection, pneumothorax | Thoracic surgery T5/6, chole/renal T8-12 Avoid lateral angulation |
| Intercostal nerve block | Open chole/fractured ribs | Rib angle (immediately lateral to the erector spinae muscles) | Insert needle perpendicular to skin downwards on inferior rib border, walk off & insert 2-5 mm | LOR | 5 ml 0.5% Levobupivicaine | Pneumothorax, absorption toxicity, intravascular injection |
Lower Limb Peripheral Nerve Blocks
| Block | Indications | LM | Technique | Stim/end point | LA | SE/Complications | Clinical points |
|---|---|---|---|---|---|---|---|
| Penile block | Circumcision | Symphysis pubis, mark 2 points 0.5-1 cm either side of the midline just below the SP | Posterior, medial and slightly caudal until LOR (elastic recoil with Buck’s fascia). Infiltrate subQ around penile root onto lateral side of the scrotum | 8-30 mm | 5 ml 0.5% Levobupivicaine | Puncture corpus cavernosum/dorsal vessels | By infiltrating laterally you can get branches of the ilioinguinal and iliohypogastric nerves |
| Ilioinguinal/iliohypogastric nerve blocks | Inguinal surgery including orchidopexy | ASIS, Deep inguinal ring (1-1.5 cm above midinguinal point) | 2 cm medial to ASIS (1 cm in children) | Ilioinguinal: initial click Iliohypogastric: 2nd click Intercostal nerves: fan out SubQ infiltration | 10 ml 0.5% Levobupivicaine 5-10 ml 0.5% Levobupivicaine | Intravascular, intraperitoneal injection, femoral nerve block | Tell patient about femoral nerve block |
| Caudal (children) | Circumcision, orchidopexy, herniotomy, anaesthesia for LLs | PSIS, Sacral cornu, Sacral hiatus | Palpate PSIS, the hiatus is at the apex of an equilateral triangle whose base is formed by a line linking the two PSIS. Or, palpate the cornu, the depression between them & immediately inferior is the hiatus | 22g needle, cephalad 45 degrees in children, (15 degrees in babies – sacrum flatter). Pop felt as sacrococcygeal membrane is perforated | Depends on level of operation – LS 0.5 ml/kg TL 1.0 ml/kg Mid thoracic 1.25 ml/kg of 0.25% Levobupivicaine | ||
| Lumbar plexus block | NOF, femoral shaft, TKR, all leg/foot surgery (with sciatic) | Line parallel to spinous processes passing through PSIS. Mark where this crosses Tuffier’s line | Perpendicular to skin, slightly caudal, contact transverse process, then re-direct above/below TP – depth 10-12 cm | Quadriceps contraction | 20 ml 0.5% Levobupivicaine | Epidural spread, intravascular, bleeding | Hamstrings – too medial/caudal Avoid too medial -> epidural spread |
| Sacral plexus block | Hip surgery, post amputation (also, see indications for sciatic n. block) | PSIS, ischial tuberosity | Draw a line from PSIS to IT, at a point 6 cm distal to the PSIS. Perpendicular to skin, contact bone and redirect caudally and advance 2 cm (depth 60-80 mm) | Plantar flexion of foot/toes (tibial n.) | 10-20 ml 0.5% levobupivicaine | Perforation pelvic viscera, intravascular injection. Blockade of other components of sacral plexus. | Eversion of foot (move medially). Sacral parasympathetics can be blocked –> urinary retention. |
| Sciatic nerve block | Solely – ankle/foot surgery. With femoral n. – amputation, knee surgery. | PSIS, greater trochanter, IT. | Flex knee to 90 degrees, draw a line connecting GT & IT, mark a point half way in the groove between the hamstrings & adductors | Plantarflexion of foot/toes (tibial n.) | 10-20 mls 0.5% levobupivicaine | Vascular puncture, intravascular injection | Eversion of foot (move medially). |
| Femoral nerve block | Solely – knee surgery, femoral shaft fracture. | Inguinal ligament, femoral artery. | 1 cm below & 1 cm lateral to the femoral artery, 30-50 mm | Patellar twitch | 10-20 mls 0.5% levobupivicaine | Vascular puncture, intravascular injection | Sartorius too superficial |
| Lateral cutaneous nerve of thigh | Hip/femoral surgery | ASIS, inguinal ligament | 2 cm medial/2 cm inferior to ASIS, infiltrate above & below fascia lata (click felt) | 10 ml 0.5% Levobupivicaine | Femoral n. block | ||
| Knee/popliteal block | Ankle/foot surgery | Apex and borders of the popliteal fossa | Mark a point 1 cm lateral to the midline & 6-8 cm proximal to the crease | Tibial: plantar flexion Common peroneal: dorsiflexion/eversion | 10-15 ml 0.5% Levobupivicaine | Vascular puncture | Work laterally to find common peroneal nerve |
| Saphenous nerve block | Ankle/foot surgery in addition to popliteal block | Tibial tubercle to medial condyle of tibia | Infiltrate subcutaneously | 10-20 mls 0.25% levobupivicaine | Bleeding (long saphenous vein) | ||
| Ankle block | Forefoot & toe surgery | DP, posterior tibial artery, medial malleolus, sustentaculum tali | Deep fibular n: 2-3 cm distal to inter-malleolar line, either side of the DP Superficial fibular n: from above point, infiltrate subQ across the dorsum of the foot. Tibial n: posterior to tibial posterior artery (midway between MM & calcaneum) Sural n: infiltrate from LM to lateral border of achilles tendon | 2 ml 0.5% Levobupivicaine each side 5-10 ml 0.5% Levobupivicaine 5-8 ml 0.5% Levobupivicaine 5 ml 0.5% Levobupivicaine | |||
| Midtarsal block | Minor surgery of toes/forefoot | MTPJ | 2 cm proximal to the MTPJ, insert needle to plantar aspect of foot | 6-8 ml 0.5% Levobupivicaine | Haematoma | No appreciable motor block |
Regional Anaesthesia in Patients on Anticoagulation
Comparison Between the ASRA Regional Anesthesia and Pain Guidelines
General Recommendations
- All previous ASRA guidelines, including the current fourth edition, do not recommend discontinuation of aspirin or NSAIDs prior to the placement of epidural and spinal blocks.
- The guidelines do not differentiate between interventional pain procedures and perioperative regional anesthesia blocks, needle/catheter trauma, degree of anticoagulation, and ability to compress the site.
- ASRA guidelines may be appropriate for low or intermediate-risk categories, but high-risk procedures require a more conservative approach.
Aspirin and NSAIDs Management
- Aspirin and NSAIDs may be continued for low-risk pain procedures.
- For mediumand high-risk procedures, antiplatelet therapy is discontinued.
- Discontinuation Length for Aspirin:
- Primary Prevention (no overt cardiovascular disease): 6 days
- Secondary Prophylaxis: 4 days
- Discontinuation Length for NSAIDs:
- 1 to 2 days: Ibuprofen, diclofenac, ketorolac, indomethacin
- 4 days: Naproxen, meloxicam
- 6 days: Nabumetone
- 10 days: Oxaprozin, piroxicam
- Discontinuation Length for Aspirin:
- Aspirin and NSAIDs can be resumed a day after the procedure.
Potent Antiplatelet Agents
- There is no significant difference between the guidelines in managing more potent antiplatelet agents, including clopidogrel, ticlopidine, ticagrelor, and prasugrel.
Heparin Management
- Regional guidelines allow neuraxial injections in patients receiving SC BID heparin.
- Pain guidelines prefer that moderate and high-risk procedures not be performed.
- If an interventional procedure is indicated, an interval of 6 hours (rather than 4-6 hours) should be followed.
Timing Intervals for Neuraxial Injection
- Regional anesthesia guidelines recommend a 4 to 6-hour interval between administration of the drug and neuraxial injection.
- Pain guidelines recommend an interval of 6 hours.
LMWH, Warfarin, Thrombolytic Therapy, and Fondaparinux
- The guidelines on LMWH, warfarin, thrombolytic therapy, and fondaparinux are the same for both regional anesthesia/acute pain and interventional pain patients.
Procedural Anticoagulation Management Checklist
1. Evaluate Baseline Patient-Specific Risk Factors for Perioperative Bleeding
- History and physical examination signs suggestive of a bleeding disorder:
- History of unexplained nosebleeds (epistaxis) or menorrhagia
- Examination signs including petechiae, mucosal bleeding, purpura, or ecchymoses
- Family history of bleeding disorders.
- Screen for antiplatelet, antithrombotic, or thrombolytic therapy.
- Screen for SNRIs, SSRIs, and herbal therapies that may influence coagulation status.
- Order coagulation tests when needed based on history and physical examination and/or medication use.
- Identify aspirin and non-aspirin NSAIDs utilization.
2. For Individuals on Aspirin Categorize Reason for Utilization
- Primary prophylaxis → absence of established cardiovascular disease or risk factor.
- Secondary prophylaxis → presence of cardiovascular disease.
3. Process the Anatomical Location of Procedural Intervention into Decision-Making
- Intracanal vs extracanal spinal procedures
- Cervicothoracic neuraxial area or lumbosacral neuraxial area.
- Surrounding vascular structures at risk for penetration.
4. Review Appropriate Radiographic Imaging to Identify and Understand Anatomic Challenges
- Cervical, thoracic, and lumbar spinal stenosis that alter spinal canal anatomy
- Epidural fibrosis and significant scar tissue from previous surgical intervention
5. Identify and Manage Pharmacologic Coagulopathies
- Understand drug elimination and appropriate discontinuation time.
- Determine appropriate timing for reinitiation of anticoagulation and antiplatelet therapy.
- Practice informed decision-making involving procedural physician, prescribing medical physician, and patient.
6. Employ Post-Procedure Surveillance for the Detection of Bleeding Complications
Stratification of Risk According to Procedures
Low Risk
Regional Guidelines:
- Superficial and compressible plexus/peripheral nerve blocks
Pain Guidelines:
- Peripheral nerve blocks
- Joint injections
- Sacroiliac joint and sacral lateral branch blocks
Intermediate Risk
Regional Guidelines:
- Other procedures based on compressibility, patient body habitus, comorbidities, and the degree and duration of anticoagulation
Pain Guidelines:
- Neuraxial injections
- Facet procedures
- Visceral sympathetic blocks
- Pocket revision
High Risk
Regional Guidelines:
- Neuraxial blocks
- Deep and noncompressible plexus/peripheral nerve blocks
Pain Guidelines:
- Spinal cord stimulator trial and implant
- Intrathecal pump trial and implant
- Vertebroplasty and kyphoplasty
- Epiduroscopy
Recommendations for Thromboprophylaxis in Nonorthopedic Surgical Patients
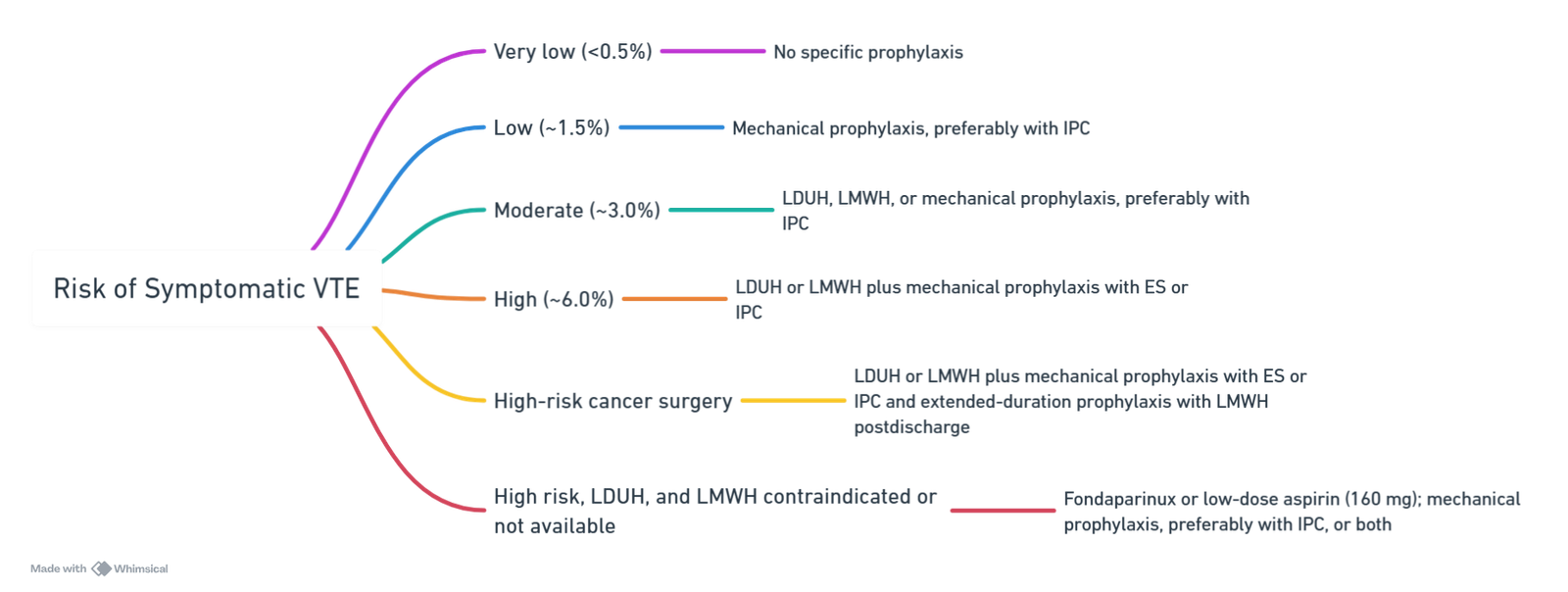
View or edit this diagram in Whimsical.
Warfarin
ASRA Guidelines for Neuraxial Techniques and Warfarin Therapy
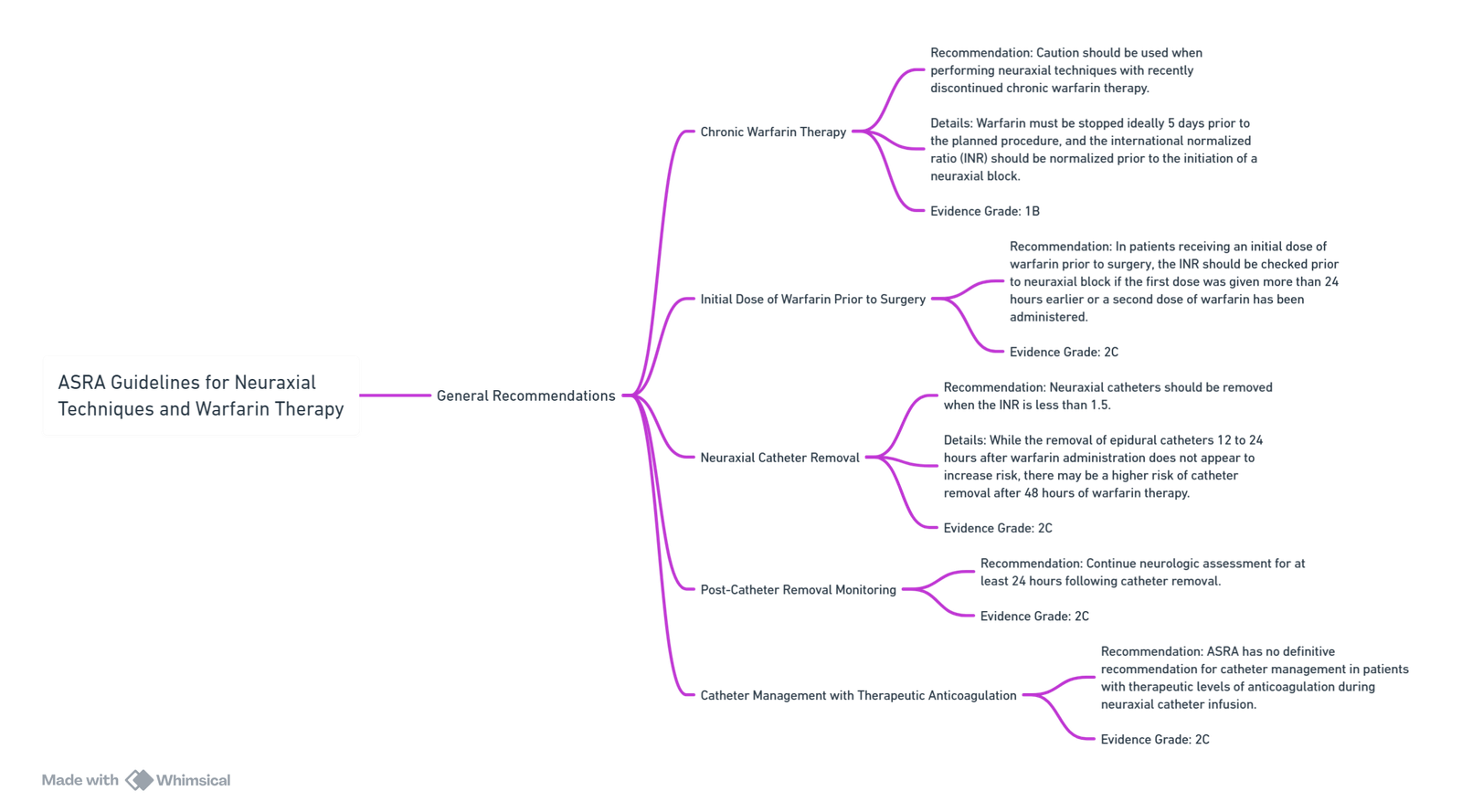
View or edit this diagram in Whimsical.
Patient Characteristics Associated With Increased Sensitivity to Warfarin
- Age >65 y
- Female sex
- Weight <100 lb
- Liver, cardiac, or renal disease
- Asian ancestry
- Excessive surgical blood loss
Half-lives of Vitamin K–Dependent Clotting Factors
| Factor | Half-Life (h) |
|---|---|
| Factor VII | 6–8 |
| Factor IX | 24 |
| Factor X | 25–60 |
| Factor II | 50–80 |
Perioperative Management of Patients on Warfarin
Preoperative
- Discontinue warfarin at least 5 days before elective procedure
- Assess INR 1–2 d prior to surgery, if >1.5, consider 1–2 mg oral vitamin K
- Reversal for urgent surgery/procedure, consider 2.5–5 mg oral or IV vitamin K; for immediate reversal, consider PCCs, fresh frozen plasma
- Patients at high risk of thromboembolism
- Bridge with therapeutic SC LMWH (preferred) or IV UFH
- Last dose of preoperative LMWH administered 24 h before surgery, administer half of the daily dose
- Intravenous heparin discontinued 4–6 h before surgery
- No bridging necessary for patients at low risk of thromboembolism
Postoperative
- Patients at low risk of thromboembolism
- Resume warfarin on POD
- Patients at high risk of thromboembolism (who received preoperative bridging therapy)
- Minor surgical procedure—resume therapeutic LMWH 24 h postoperatively
- Major surgical procedure—resume therapeutic LMWH 48–72 h postoperatively or administer low-dose LMWH
- Assess bleeding risk and adequacy of hemostasis when considering timing of the resumption of LMWH or UFH therapy
Links
- Upper limb blocks
- Lower limb blocks
- Anticoagulation|Anticoagulation
- Anticoagulation and blocks
- Obstetrics Anticoagulation|Obstetrics Anticoagulation
References:
- Wai, C. L. W. and Irwin, M. G. (2012). Regional blocks in orthopaedics. Anaesthesia &Amp; Intensive Care Medicine, 13(3), 89-93. https://doi.org/10.1016/j.mpaic.2011.12.004
- Horlocker, T. T., Vandermeuelen, E., Kopp, S. L., Gogarten, W., Leffert, L., & Benzon, H. T. (2019). Regional anesthesia in the patient receiving antithrombotic or thrombolytic therapy: american society of regional anesthesia and pain medicine evidence-based guidelines (fourth edition). Obstetric Anesthesia Digest, 39(1), 28-29. https://doi.org/10.1097/01.aoa.0000552901.03545.fb
- Checketts, M. R. (2016). Intravenous regional anaesthesia. Anaesthesia &Amp; Intensive Care Medicine, 17(4), 192-193. https://doi.org/10.1016/j.mpaic.2015.12.013
- FRCA Mind Maps. (2024). Retrieved June 5, 2024, from https://www.frcamindmaps.org/
- Anesthesia Considerations. (2024). Retrieved June 5, 2024, from https://www.anesthesiaconsiderations.com/
- Boutique Workshops. (n.d.). In NYSORA. Retrieved June 26, 2024, from https://www.nysora.com/mec-category/boutique-workshops/
- ASRA Pain Medicine. (n.d.). Guidelines. Retrieved June 27, 2024, from https://www.asra.com/guidelines-articles/guidelines
- European Society of Regional Anaesthesia & Pain Therapy (ESRA). (n.d.). Guidelines. Retrieved June 27, 2024, from https://esraeurope.org/guidelines/
- Teaching videos
Summaries:
Analgesia for hips and knees
Brachial plexus blocks
Lower limb blocks
Elbow and wrist blocks
Ultrasound for regional anaesthesia
Paravertebral blocks
Regionals for hip fractures
Epidural benefits
Anterior abdominal wall nerve blocks
LAST
Epidural connectors
Copyright
© 2025 Francois Uys. All Rights Reserved.
id: “33f7fb5d-37f2-4fad-9646-a72e6ec46e44”



