{}
Anatomy
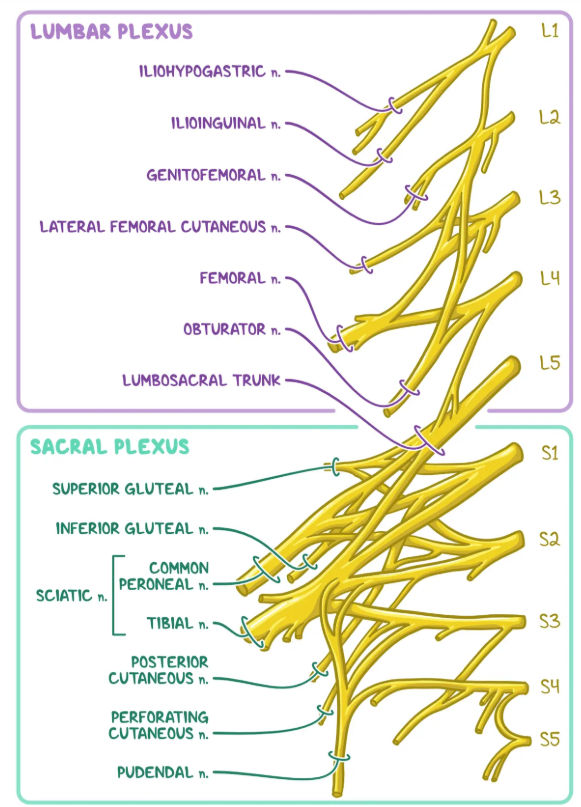
Lumbosacral Plexus–Clinical Anatomy for Lower-Limb Blocks
| Plexus | Roots | Formation & Course | Key Motor / Sensory Branches | Block(s) that target it |
|---|---|---|---|---|
| Lumbar plexus | T12–L4 (occasionally T11) | Forms within substance of psoas major; roots emerge between its fascicles, then exit lateral, anterior or medial to the muscle | • Iliohypogastric (T12–L1)–suprapubic sensation • Ilioinguinal (L1)–groin, upper scrotum/labium • Genitofemoral (L1–L2)–cremaster, upper anterior thigh • Lateral femoral cutaneous (L2–L3)–anterolateral thigh • Femoral (L2–L4)–quadriceps, skin anteromedial thigh & leg (saphenous) • Obturator (L2–L4)–hip adductors, medial thigh skin • Lumbosacral trunk (L4–L5)–joins sacral plexus |
Lumbar plexus / psoas compartment; supra-inguinal fascia-iliaca; femoral; adductor-canal; obturator; lateral cutaneous nerve block |
| Sacral plexus | L4–S4 (L4–L5 via lumbosacral trunk + S1–S4 ventral rami) | Lies on anterior surface of piriformis within pelvis; exits via greater sciatic foramen beneath piriformis | • Superior gluteal (L4–S1)–gluteus medius/minimus • Inferior gluteal (L5–S2)–gluteus maximus • Posterior femoral cutaneous (S1–S3)–posterior thigh • Sciatic (L4–S3)–divides to tibial (L4–S3) & common peroneal (L4–S2) • Pudendal (S2–S4)–perineum • Nerve to obturator internus / quadratus femoris |
Parasacral & sub-gluteal sciatic; popliteal sciatic; ankle (terminal branches); sacral plexus block |
| Tibial division of sciatic | L4–S3 | Runs in posterior thigh with hamstrings → popliteal fossa, continues deep to soleus as posterior tibial nerve | Motor: posterior compartment of leg & plantar foot Sensory: sole (medial & lateral plantar), heel (medial calcaneal), sural (lateral foot with CP contribution) |
Popliteal (proximal), ankle tibial, mid-tarsal |
| Common peroneal (fibular) division | L4–S2 | Lateral popliteal fossa → winds round fibular neck → branches superficial & deep peroneal | Motor: anterior & lateral compartments (dorsiflexors, evertors) Sensory: dorsum of foot (superficial), first web-space (deep) |
Popliteal, ankle deep & superficial peroneal |
| Saphenous (terminal femoral) | L3–L4 | Within adductor canal then sub-cutaneous medial leg to great toe | Pure sensory–medial leg, ankle & foot arch | Adductor-canal, distal saphenous ring |
| Posterior femoral cutaneous | S1–S3 | Exits pelvis with sciatic, lies medial to it | Sensory–posterior thigh, popliteal fossa | Rarely blocked alone; incidentally with sciatic / sacral plexus |
Functional Themes for Block Planning
- Anterior thigh & knee–femoral or supra-inguinal fascia-iliaca (captures femoral ± LFCN ± obturator depending on spread).
- Medial thigh & hip adductors–obturator.
- Hip joint–dual lumbar & sacral supply → combine lumbar plexus or supra-inguinal fascia-iliaca with sciatic (parasacral) for complete analgesia.
- Knee arthroplasty–adductor-canal (sensory-sparing motor) ± IPACK (posterior capsule) covers most innervation while preserving quadriceps.
- Foot & ankle–popliteal sciatic (tibial + common peroneal before division) + saphenous for medial ankle; ankle five-nerve block for distal procedures without proximal motor weakness.
- Understanding the plexus topology (roots → plexus → division → terminal nerve) explains why:
- high-volume supra-inguinal fascia-iliaca can reach obturator and LFCN, whereas inguinal approaches often miss them;
- sacral plexus or proximal sciatic blocks are required for posterior hip/knee structures that lumbar plexus blocks cannot cover;
- distal adductor-canal blocks spare quadriceps because motor branches to vastus muscles leave the femoral nerve proximally within the thigh.
Innervation
Hip
- Femoral nerve–nerve to rectus femoris
- Sciatic nerve–nerve to quadratus femoris
- Obturator nerve–anterior division
Knee
- Femoral nerve–branch to vastus medialis
- Sciatic nerve–tibial & common peroneal branches
- Obturator nerve–posterior branch
Lower Limb Blocks
| Approach (US-guided) | Plexus / nerve level | Usual LA volume | Typical operations (evidence-based) | Tourniquet cover | Specific complications(best-estimate incidence) | Key caveats | Landmark / probe position | Needle technique | Motoror sensory stim end-point |
|---|---|---|---|---|---|---|---|---|---|
| Lumbar plexus (psoas compartment) | L1–L4 plexus | 20–30 mL | Hip replacement, fracture NOF (with sciatic for full limb), major knee | Thigh | Epidural spread (5–15 %) · Retroperitoneal haematoma (<0.1 %) | Deep block; anticoagulation caution | Curved probe transverse at L3–L4, 4 cm lateral to spinous line | In-plane lateral→medial to psoas groove | Quadriceps twitch / patellar snap < 0.5 mA |
| Fascia-iliaca (supra-inguinal) | Femoral ± LFCN | 30–40 mL | Hip fracture analgesia, THR, paediatric femur surgery | Thigh partial | Quadriceps weakness → falls (4 %) | Spread unpredictable distal to knee | Linear probe parasagittal, just medial to ASIS under fascia iliaca | In-plane caudad→cephalad; hydro-dissect deep to fascia | Absent twitch acceptable (pure US) |
| Femoral nerve | L2–L4 nerve | 15–20 mL | ACL repair, TKA (single-shot), femoral shaft fracture | Thigh partial | Vascular puncture (2–8 %) · Post-op falls (1–3 %) | Avoid large volumes in anticoagulated pts | Linear probe at femoral crease, visualise nerve lateral to artery | In-plane lateral→medial; inject beneath fascia iliaca | Patellar lift / quadriceps twitch < 0.5 mA |
| Adductor canal (saphenous) | Saphenous ± nerve-to-VM | 10–15 mL | Analgesia after TKA, knee arthroscopy, ankle surgery (with sciatic) | Thigh partial | Sensory-only block–quadriceps strength preserved (> 90 %) | Ideal for early mobilisation | Linear probe mid-thigh, artery beneath sartorius | In-plane lateral→medial; LA around artery | Paresthesia over medial calf (rare) |
| Obturator nerve | L2–L4 anterior & posterior branches | 8–10 mL | Medial knee arthroplasty, TURBT obturator reflex prevention | None | Vascular puncture (< 2 %) · Bladder puncture (< 0.1 %) | Use with GA during TURBT | Linear probe proximal thigh, medial to femoral vessels | Out-of-plane; 2 injections between adductor muscles | Adductor thigh twitch < 0.5 mA |
| Sciatic–sub-gluteal / parasacral | L4–S3 plexus | 20–25 mL | THR (with femoral), hamstring or posterior knee surgery | Thigh | Foot-drop neuropraxia (0.2 %) · Vascular puncture (1 %) | Careful positioning to avoid sciatic stretch | Curved probe posterior gluteal fold, greater trochanter ↔ ischial tuberosity | In-plane lateral→medial to nerve | Plantar flex (tibial) / dorsiflex (peroneal) < 0.5 mA |
| Popliteal sciatic (prox + distal) | Sciatic division before bifurcation | 20–25 mL | Foot & ankle surgery, Achilles repair | Calf | Transient peroneal neuropathy (0.3 %) | Combine with saphenous for medial ankle | Linear probe 6–8 cm above popliteal crease | In-plane lateral→medial; circumferential LA | Tibial: plantar flex; CP: dorsiflex < 0.5 mA |
| Saphenous (distal) | Saphenous nerve | 5–10 mL | Medial ankle / foot surgery (with popliteal) | None | Long saphenous vein puncture (≤ 1 %) | Purely sensory–no motor weakness | Linear probe medial tibial condyle → mid-leg | Subcutaneous ring infiltration | No stim target (sensory) |
| Ankle block (5-nerve) | Terminal branches | 20–25 mL total | Forefoot / toe surgery, hallux valgus | None | Vascular puncture (dorsalis pedis ≈ 3 %) | Minimal motor block–ambulation preserved | Landmark or linear probe around malleoli | Multiple Infiltrations: DP, tibial, sural, superficial & deep peroneal | Not applicable–sensory cutaneous nerves |
Motor-sparing” Regional Techniques now Favoured for Total Knee Arthroplasty (TKA)
| Sensory targets covered | Technique (LA ≤ 20 mL unless stated) | Quadriceps or foot strength affected? | Key evidence for motor-sparing benefit |
|---|---|---|---|
| Anterior & medial capsule + infrapatellar skin • Saphenous n. • Nerve to vastus medialis |
Adductor-canal block (ACB) or the slightly more proximal Femoral-triangle block (single-shot 15 mL or continuous catheter at 6 mL h⁻¹) | No clinically relevant loss of quadriceps force (≈ 5 % vs 30-50 % with femoral-nerve block) | Randomised trials & 2024 scoping review confirm preserved Timed-Up-and-Go and earlier mobilisation with analgesia non-inferior to femoral block |
| Posterior capsule | IPACK block (Infiltration between the Popliteal Artery and Capsule of the Knee) 15–20 mL via medial in-plane approach at femoral condyles | Spares tibial & peroneal motor fibres; plantarand dorsiflexion unchanged | Narrative review 2023 and multiple RCTs show better early mobilisation and opioid-sparing when IPACK is added to ACB, without motor deficit |
| Whole peri-articular soft-tissue field | Local infiltration analgesia (surgeon-delivered) ± posterior capsular injection | None (soft-tissue rather than nerve block) | Structured review notes that combining peri-articular infiltration with ACB or IPACK gives additive analgesia without any motor cost |
Whole Peri-articular Soft-tissue Field
- The “whole peri-articular soft-tissue field” strategy refers to comprehensive Local Infiltration Analgesia (LIA)—a high-volume, dilute, surgeon-directed infiltration of the joint capsule, ligaments and subcutaneous tissues (often augmented by a brief catheter infusion). It is the recommended motor-preserving supplement to adductor-canal and IPACK blocks in enhanced-recovery knee arthroplasty protocols.
| Element | Practical recommendation (current evidence-based practice) | Why it helps |
|---|---|---|
| Timing | Infiltrate intra-operatively in three stages: ① posterior capsule before implant cementing, ② collateral-ligament gutters & arthrotomy edges, ③ subcutaneous layer just before skin closure. | Posterior-first sequence bathes the most painful area before prosthesis limits access; staged dosing keeps systemic LA levels lower. |
| Mixture / dose | High-volume, dilute LA 150–170 mL e.g. ropivacaine 0.2 % (≤ 3 mg kg⁻¹ total) ± adrenaline 1:200 000 plus ketorolac 30 mg (or 0.5 mg morphine) per knee. | Large volume spreads through all nociceptor-rich tissues; adrenaline prolongs block & curbs peak blood levels; intra-articular NSAID gives added anti-inflammatory effect. |
| Optional catheter | Place an intra-articular (posterior) catheter and give 10–15 mL of the same solution every 8–12 h, or run 5 mL h⁻¹ for 24–48 h. | Continuous LIA matched femoral + sciatic catheter analgesia in a 2025 RCT while preserving full quadriceps power. |
| Posterior-capsule emphasis | Ensure at least 50 mL reaches the posteromedial & posterolateral capsule (or add an IPACK block if surgeon access is limited). | The posterior capsule is the dominant pain generator once anaesthetic wears off; targeted infiltration or IPACK prevents “back-of-knee” escape pain. |
| Compression bandage | Apply a snug elastic bandage from mid-thigh to mid-calf for 4–6 h. | Slows vascular wash-out, prolonging intra-articular drug dwell-time; reduces postoperative oozing. |
| Safety checks | Record total LA dose (ideal-body-weight basis); avoid high-concentration bolus; monitor for LAST in recovery. | Large total volumes are safe when dilute, but vigilance needed in elderly or low-BMI patients. |
Clinical Impact
- Randomised trials and a 2025 prospective study show LIA (single-shot ± catheter) delivers pain scores and opioid consumption equivalent to femoral + sciatic blocks, yet with no measurable quadriceps weakness or falls risk.
- When paired with an adductor-canal block (for anterior capsule) or an IPACK block (if posterior infiltration is sub-optimal), LIA forms the core of modern motor-sparing multimodal pathways for total knee arthroplasty.
Ankle block—overview of the “five-nerve” Technique
| Nerve (root) | Cutaneous / surgical territory anaesthetised | Landmark & needle path | Typical LA volume |
|---|---|---|---|
| Tibial (L4–S3) | Sole of foot, plantar toes, nail beds | Palpate posterior tibial artery just posteroinferior to the medial malleolus; insert needle immediately posterior to artery → advance 0.5–1 cm until paresthesia / loss of resistance in flexor retinaculum | 3–5 mL |
| Deep peroneal (L4–S1) | Dorsum of first web-space (1st–2nd toes) | At ankle crease between the tendons of extensor hallucis longus (medial) & extensor digitorum longus (lateral); advance to periosteum of talus | 2–3 mL |
| Superficial peroneal (L4–S1) | Most of dorsum of foot & toes (except first web-space) | Subcutaneous ring infiltration from mid-tibia crest to lateral malleolus across anterior ankle | 5–7 mL (fan) |
| Sural (S1–S2) | Lateral foot & fifth toe | Posterior to lateral malleolus at Achilles–calcaneal junction; infiltrate subcutaneously towards the fibula | 3–5 mL |
| Saphenous (L3–L4) | Medial foot from malleolus to first metatarsal head | Subcutaneous wheal anterior to medial malleolus along tibial border | 3–5 mL |
- Volumes assume a 0.5 % ropivacaine or 1 % lidocaine solution; adjust to weight limits and concentration.
Step-by-step Technique (supine Patient, Foot Slightly everted)
- Preparation–Full aseptic prep, 25 G × 38 mm needle, draw up total 15–20 mL of LA.
- Tibial nerve first–aids analgesia during subsequent injections.
- Deep peroneal nerve–confirm position by dorsiflexion of big toe (tendon identification).
- Superficial peroneal–raise a subcutaneous fan across the anterior ankle.
- Sural nerve–single depot posterolateral to lateral malleolus.
- Saphenous nerve–subcutaneous fan anterior-medial to malleolus.
- Assess–Onset 10–20 min; check with cold or pin-prick before incision
Practical Pearls & Cautions
- Motor sparing: only minor toe flexion/extension weakness → ideal for ambulatory foot surgery.
- Vascular proximity: aspirate before tibial and deep peroneal injections (posterior tibial & dorsalis pedis arteries).
- Avoid compartment injection by using low resistance and slow deposition.
- Tourniquet pain is not covered; use separate saphenous-proximal or regional block if required above ankle.
Suggested Standard Monitoring for Nerve Blocks
Ultrasound + Nerve Stimulation + Opening Injection Pressure (OIP)
- Connect needle to nerve stimulator (0.5mA, 0.1msec, 2Hz)
- Advance needle towards the nerve or plexus
- Needle adequately placed as seen on US
- No twitch
- 1-2 mL injection of LA results in adequate spread in the desired tissue plane OIP normal <15psi
- Needle adequately placed as seen on US
- Twitch present
- Reposition the needle to assure NO twitch present at <0.5mA
- 1-2 mL injection of LA results in adequate spread in the desired tissue plane OIP normal <15psi
- Needle adequately placed as seen on US
- Complete injection
- Increase current to 1.5mA
- Adjust needle placement by US
Evidence-based Benefits of Common Lower-Limb Blocks
| Block (single-shot unless stated) | Operations with proven benefit* | Key outcome advantages (vs control / comparator) | Representative high-quality evidence |
|---|---|---|---|
| Lumbar plexus (psoas compartment) | Total hip arthroplasty, fracture neck of femur (with sciatic) | ↓ 24 h morphine 18 mg; ↓ pain ≥ 3 cm V A S; earlier independent ambulation day 2 | Randomised controlled trial, 84 pts, THA 2023 |
| Supra-inguinal fascia-iliaca block | Hip fracture fixation, primary hip replacement | ↓ 24 h opioid 22 mg OME; ↓ pain scores at 6–24 h; fewer PONV episodes | Systematic review & meta-analysis of 12 RCTs, 2024 |
| Femoral nerve block | ACL repair, single-bundle TKA | ↓ early pain but quadriceps weakness → higher fall risk | Network meta-analysis knee analgesia 2024 |
| Adductor canal block (single) | Unicompartmental & total knee arthroplasty | Similar pain to femoral block but quadriceps strength 30 % higher; 30 m ambulation distance ↑ | Meta-analysis 36 studies, 2024 |
| Continuous adductor canal block | TKA fast-track pathways | ↓ hospital stay 0.5 day; ↑ Timed-Up-and-Go performance; similar opioid to continuous femoral | Updated meta-analysis 2023 |
| Obturator nerve block | TURBT on lateral wall | Obturator reflex rate ↓ from 76 % → 6 %; bladder perforation ↓ 8 % → 0 % | Prospective RCT, 60 pts, 2022 |
| Sub-gluteal / parasacral sciatic | Hip arthroplasty (with femoral), hamstring repair | ↓ post-op morphine 25 mg; better first-night sleep quality | Prospective comparative cohort, 2021 |
| Popliteal sciatic block | Foot & ankle ORIF, Achilles rupture repair | Analgesia ≥ 18 h; rescue opioid ↓ 40 %; 0.25 % ropivacaine non-inferior to 0.375 % | Double-blind non-inferiority RCT, 2025 |
| Ambulatory continuous popliteal | Out-patient bunionectomy, calcaneal osteotomy | Non-inferior pain vs single-shot, but satisfaction ↑ and night pain ↓ | Multicentre RCT, 2024 |
| Saphenous (adductor canal distal) | Medial ankle / foot with popliteal | Adds 6 h sensory cover to medial foot without motor loss | Randomised crossover study, 2020 |
| Ankle 5-nerve block | Hallux valgus, toe arthrodesis | ↓ rescue opioid 35 %; ↓ PONV; no motor weakness → earlier discharge | PROSPECT systematic review 2019 |
Links
References:
- Wai, C. L. W. and Irwin, M. G. (2012). Regional blocks in orthopaedics. Anaesthesia &Amp; Intensive Care Medicine, 13(3), 89-93. https://doi.org/10.1016/j.mpaic.2011.12.004
- Horlocker, T. T., Vandermeuelen, E., Kopp, S. L., Gogarten, W., Leffert, L., & Benzon, H. T. (2019). Regional anesthesia in the patient receiving antithrombotic or thrombolytic therapy: american society of regional anesthesia and pain medicine evidence-based guidelines (fourth edition). Obstetric Anesthesia Digest, 39(1), 28-29. https://doi.org/10.1097/01.aoa.0000552901.03545.fb
- Checketts, M. R. (2016). Intravenous regional anaesthesia. Anaesthesia &Amp; Intensive Care Medicine, 17(4), 192-193. https://doi.org/10.1016/j.mpaic.2015.12.013
- Ahmed A, Zhang P, et al. Efficacy of continuous lumbar plexus blockade after total hip arthroplasty: randomised trial. Anaesthesia 2023;78:1124-33.
- Wang H, Li Y, et al. Ultrasound-guided supra-inguinal fascia-iliaca block for hip surgery: systematic review and meta-analysis. Pain Pract 2024;24:355-66.
- Xu D, O’Donnell R, et al. Femoral versus adductor-canal block for knee arthroplasty: network meta-analysis. Anesthesiology 2024;140:621-35.
- Deng W, Huang J. Continuous adductor canal versus femoral catheter after TKA: updated meta-analysis. J Orthop Surg Res 2023;18:411.
- Toktas C, Öztürk A, et al. Ultrasound-guided obturator block suppresses reflex during TURBT: randomised study. Urol Surg 2022;9:167-74.
- Patel S, Maddineni S. Analgesic impact of parasacral sciatic block in hip arthroplasty. Reg Anesth Pain Med 2021;46:798-804.
- Lee S, Park J, et al. 0.25 % vs 0.375 % ropivacaine for popliteal sciatic block: non-inferiority RCT. BMC Anesthesiol 2025;25:29.
- Bennett V, Gadsden J, et al. Ambulatory continuous popliteal block versus single-shot for foot surgery. Anaesth Crit Care Pain 2024;44:101-8.
- Fraser G, Nunes M. Distal saphenous block enhances popliteal anaesthesia for ankle surgery. SAJAA 2020;26:42-8.
- PROSPECT Working Group. Post-operative pain management for hallux valgus repair: systematic review. Br J Anaesth 2019;123:e129-38.
- FRCA Mind Maps. (2024). Retrieved June 5, 2024, from https://www.frcamindmaps.org/
- Anesthesia Considerations. (2024). Retrieved June 5, 2024, from https://www.anesthesiaconsiderations.com/
- Boutique Workshops. (n.d.). In NYSORA. Retrieved June 26, 2024, from https://www.nysora.com/mec-category/boutique-workshops/
- ASRA Pain Medicine. (n.d.). Guidelines. Retrieved June 27, 2024, from https://www.asra.com/guidelines-articles/guidelines
- European Society of Regional Anaesthesia & Pain Therapy (ESRA). (n.d.). Guidelines. Retrieved June 27, 2024, from https://esraeurope.org/guidelines/
- Teaching videos
Summaries:
Femoral triangle block
iPack block
Popliteal sciatic block
Suprainguinal Facia Iliaca (SIFI) or https://www.youtube.com/watch?v=ZB2REz5TTZ8
Analgesia for hips and knees
Lower limb blocks
Regionals for hip fractures
Copyright
© 2025 Francois Uys. All Rights Reserved.
id: “be71642b-b7e3-4b91-a31f-9e11daf9c2a3”



