- Types of Blocks
- Expanded Review
- Links
- Past Exam Questions
{}
Types of Blocks
- Paravertebral block (PVB)
- Erector spinae plane block (ESP)
- Serratus anterior plane block (SAPB)
- Pectoral plane blocks (PECs I and II)
- Rectus sheath block (RSB)
- Transversus abdominal plane (TAP) block
- Quadratus lumborum block (QLB)
- Ilioinguinal and iliohypogastric nerve blocks
Blocks Summary
| Block (US-guided) | Target nerves / plane | Usual LA volume† | Operations with proven benefit* | Specific complications(incidence if reported) | Key caveats | Landmark & probe | Needle technique |
|---|---|---|---|---|---|---|---|
| Thoracic paravertebral (TPVB) | Mixed spinal nerves & sympathetic chain in paravertebral space | 15–20 mL per level ± catheter | Thoracotomy, VATS, mastectomy | Pneumothorax (0–0.5 %), epidural spread (5–15 %), hypotension (≈5 %) | Haemodynamic stability better than epidural | Linear/curved probe parasagittal 2–3 cm lat. to midline | In-plane (cranio-caudal), pierce superior costotransverse lig. |
| Erector spinae plane (ESPB) | Dorsal rami + paravertebral spread (T1–L3) | 20–30 mL | VATS, rib fracture, breast cancer, laparoscopic cholecystectomy | LA systemic absorption high → LAST rare; block failure (~8 %) | Easier & safer than TPVB; analgesia 3–6 dermatomes | Parasagittal probe over transverse process (T5–T9) | In-plane (cranio-caudal), inject deep to ESM |
| Pectoral plane (PECS II) | Medial/lateral pectoral, long thoracic, thoracodorsal, IC T2–4 (lateral) | 20–30 mL | Lumpectomy, mastectomy, axillary clearance | Axillary artery puncture (<1 %), pectoral haematoma (<0.5 %) | Does not block anterior (medial) breast → consider TPVB for radical > quadrantectomy | Probe parasagittal infra-clavicular | Two in-plane deposits: between pec major/minor (I) & minor/serratus (II) |
| Serratus anterior plane (SAP) | Lateral cutaneous branches T2–T9 | 25–30 mL | Mastectomy, rib fracture, thoracotomy drain pain | Pneumothorax (<0.2 %), thoracodorsal vessel injury (<1 %) | Medial breast/nipple not covered | Probe mid-axillary 4th–5th rib | In-plane superficial or deep to serratus |
| Rectus sheath block (RSB) | Anterior cutaneous T7–T12 | 15–20 mL each side | Umbilical hernia repair, paediatric pyloromyotomy | Peritoneal perforation (<0.1 %) | Purely somatic; no visceral analgesia | Probe transverse at umbilicus | In-plane lateral→medial, LA between muscle & posterior sheath |
| Transversus abdominis plane (TAP)—lateral | Anterior rami T10–L1 | 20 mL each side | Caesarean (no IT morphine), open prostatectomy, ileostomy closure | Liver/spleen puncture (<0.1 %), LAST if bilateral large volume | No visceral pain relief; limited supra-umbilical spread | Probe axial mid-axillary line, iliac crest | In-plane between IO & TA |
| TAP—oblique sub-costal | Anterior rami T6–T10 | 25 mL each side | Laparoscopic cholecystectomy, upper GI sleeve, liver resection | Same as lateral TAP | Bilateral block needed for midline | Probe parallel to costal margin | In-plane cephalad→caudad below rectus |
| Quadratus lumborum (QL)–posterior | Thoracolumbar fascia; spread to paravertebral T7–L1 | 25–30 mL | Caesarean, nephrectomy, hip arthroplasty (anterior QL) | Femoral weakness (7 %), retro-peritoneal haematoma (<0.2 %) | Longer duration but slower onset; caution bilateral high volumes | Probe posterior axillary above iliac crest | In-plane post. to QL (type 2) |
| Ilio-inguinal / ilio-hypogastric | L1 terminal branches | 10–15 mL | Open & lap inguinal hernia, Pfannenstiel incision | Peritoneal puncture (<0.5 %) | Useful rescue when TAP fails | Probe medial to ASIS | In-plane into plane IO/TA |
General Complications
- Accidental Peritoneal Puncture
- Intravascular Injection LAST
- Failure
- QLB:
- retroperitoneal hematoma, psoas weakness, femoral nerve block
- Catheters:
- infection, dislodgment, leaking, migration
Catheter Infusion Regimens
| Block | Starting rate | Typical mix | Notes |
|---|---|---|---|
| TPVB | 6–8 mL h⁻¹ | 0.2 % ropivacaine ± 2 µg mL⁻¹ clonidine | Bolus 5 mL q4 h prn |
| ESPB (T5–T7) | 8–10 mL h⁻¹ | 0.2 % ropivacaine | Safe on ward; monitor dermatomes q4 h |
| Sub-costal TAP | 6 mL h⁻¹ side⁻¹ | 0.125 % bupivacaine | Secure catheter lateral to semilunar line |
| Posterior QL | 5 mL h⁻¹ side⁻¹ | 0.2 % ropivacaine | Watch for quadriceps weakness when bilateral |
Suggested Single-Shot Dosing (lean BW)
| Block | Low-risk adult | Frail / paediatric |
|---|---|---|
| TPVB (1 level) | 0.3 mL kg⁻¹ of 0.5 % ropivacaine (max 20 mL) | 0.2 mL kg⁻¹ of 0.25 % |
| ESPB | 0.4 mL kg⁻¹ of 0.375 % | 0.3 mL kg⁻¹ of 0.25 % |
| SAP/PEC II | 0.4 mL kg⁻¹ of 0.25 % | 0.25 mL kg⁻¹ of 0.2 % |
| Sub-costal TAP | 0.3 mL kg⁻¹ side⁻¹ of 0.25 % | 0.2 mL kg⁻¹ side⁻¹ |
- All volumes split bilaterally when required.
Adjuvants
- Dexamethasone 4 mg (perineural or IV)–prolongs TPVB/TAP analgesia ≈ 8 h; avoid surgical site infection concerns.
- Dexmedetomidine 25–50 µg–increases ESPB, QLB duration by 6–8 h; monitor bradycardia.
- Clonidine 1 µg kg⁻¹–useful when dexmedetomidine unavailable.
- Epinephrine 5 µg mL⁻¹–reduces peak plasma level by one-third in TAP / ESPB (2024 kinetic study).
Anticoagulation / Bleeding-risk Guidance (ASRA-4th edition)
| Block group | Recommendation |
|---|---|
| Superficial fascial-plane (TAP, SAP, PEC) | No mandatory pause beyond standard dermal closure haemostasis; compress site 5 min. |
| Interfascial but near major vessels (QL, ESPB) | Treat as “low-to-intermediate” risk: delay 4 h after SC heparin; resume 2 h post-block. |
| TPVB / deep QL | Intermediate risk: follow neuraxial timing for DOACs (≥ 48 h off). |
Evidence
| Surgery | Best-supported block(s) | Outcome highlights (vs control) |
|---|---|---|
| Open thoracotomy | TPVB catheter | Pain scores ↓ ≥ 30 % for 48 h; hypotension 50 % less than epidural |
| VATS | ESPB single or catheter | Morphine 24 h ↓ 18 mg; ambulation earlier |
| Breast cancer surgery | TPVB > ESPB ≈ SAP + PEC II | Morphine 24 h TPVB ↓ 15 mg; ESPB ↓ 12 mg; SAP ↓ 11 mg |
| Radical mastectomy | PEC II + SAP | Non-inferior pain to TPVB but easier, fewer side-effects |
| Caesarean section (no IT morphine) | QL (posterior) | 12 h morphine ↓ 10 mg; pain at rest ↓ 2 V A S |
| Robotic prostatectomy | Bilateral sub-costal TAP catheter | Opioid 24 h ↓ 25 mg; PONV ↓ 40 % |
| Laparoscopic gynae procedures | TAP (lateral) | Very low-certainty benefit; consider port infiltration |
| Umbilical hernia repair | RSB | Pain 6 h ↓ 2 V A S; morphine ↓ 8 mg |
ERAS-Aligned Benefits
- Thoracotomy: TPVB ± ketamine infusion ↓ unplanned NIV, ↓ LOS 1 day.
- Caesarean (no IT morphine): Posterior QL + low-dose IV lidocaine ↓ time-to-first mobilisation by 3 h.
- Robotic prostatectomy: Bilateral sub-costal TAP + rectus sheath infiltration ↓ shoulder-tip pain and PONV vs port infiltration alone.
Expanded Review
Anterior Abdominal Wall Blocks
Transverse Abdominus Block
Dosing
- Concentration: No significant difference between low vs. high concentration of local anaesthetics.
- Volume: Effective analgesia requires volumes >15 ml per side.
- Dosing Strategy: Lean body weight-based dosing to prevent local anesthetic systemic toxicity (LAST).
- Delivery Method: Perineural infusion block (PIB) vs. continuous infusion.
- Absorption Kinetics: Rapid first-phase absorption with a mean time to maximum serum concentration of 10-35 minutes.
- Epinephrine Addition: Epinephrine (5 mcg/ml) reduces maximum plasma concentration by 35%.
Optimal Local Anaesthetic (LA)
- Ropivacaine vs. Bupivacaine: No significant difference in efficacy.
- Bupivacaine vs. Liposomal Bupivacaine: Insufficient evidence to determine superiority.
- Catheter Techniques: Comparison between PIB and continuous infusion, and between multiple catheters (up to 4) vs. liposomal formulations, remains inconclusive.
Block Types
| Block Type | Target | Landmarks | Indications | Limitations |
|---|---|---|---|---|
| Subcostal TAP | Anterior cutaneous branches of T6-T10 | Subcostal margin, rectus abdominis, and transversus abdominis (TA) | Unilateral, midline upper abdominal incisions (e.g., open cholecystectomy) | No visceral coverage |
| Lateral TAP | Anterior divisions of intercostal nerves T10-L1 | Internal oblique, external oblique, and triangle of Petit | Unilateral/midline lower abdominal wall incisions (e.g., hernia, ostomy, C-section) | Limited spread, no visceral coverage |
| Posterior TAP | Anterior cutaneous branches of T7-L1 | Posterior axillary line, above iliac crest, below costal margin, intersection of TA and quadratus lumborum (QL) | Abdominal surgery above or below umbilicus | Possible visceral coverage, similar to lateral QL |
| Quadratus Lumborum | T4-L1 anterior and lateral cutaneous branches | Posterior axillary line, above iliac crest, below costal margin | Abdominal surgery above or below umbilicus | Limited data, potential spread to paravertebral space/lumbar plexus (risk of quadriceps weakness) |
Additional Evidence
- Ultrasound Guidance: The adoption of ultrasound for nerve block techniques has expanded the use of the TAP block for perioperative analgesia in various abdominal surgeries, demonstrating significant efficacy in providing analgesia when combined with multimodal analgesic techniques.
- Pain and Opioid Reduction: The TAP block reduces pain scores and opioid consumption in lower-abdominal surgeries, including anterior iliac crest bone harvesting, hysterectomy, prostatectomy, cesarean section, and major upper abdominal surgeries.
- Continuous Posterior TAP Catheter: The four-quadrant TAP block with a continuous posterior TAP catheter provides comparable analgesia and postoperative pain scores, along with non-inferior rescue analgesic consumption levels compared to continuous thoracic epidural analgesia (TEA).
- Complications and Safety: Despite numerous studies confirming efficacy, choosing the best TAP block approach for specific surgical procedures remains complex. Posterior TAP blocks are recommended for incisions below the umbilicus, while subcostal or oblique subcostal TAP blocks are suggested for supraumbilical incisions. Complications are rare with ultrasound-guided TAP blocks, making them relatively simple and safe procedures. Potential complications include organ damage and systemic toxicity due to the large injection volumes required.
Rectus Sheath Block
Clinical Background and Anatomy
- Local anaesthetic (LA) is deposited in the rectus sheath beneath the rectus abdominis muscle, blocking the terminal anterior cutaneous branches of the intercostal nerves from T9 to T11. These nerves transfer sensory information from the periumbilical skin.
- Typically performed bilaterally, the rectus sheath block is widely used for analgesia in surgeries involving midline incisions.
Ultrasound-Guided Rectus Sheath Block Techniques
- Patient Position: Supine.
- Ultrasound Probe Position: Transverse over the rectus abdominis muscle.
- Equipment: High-frequency linear probe.
- Procedure: Insert the needle between the rectus abdominis muscle and the posterior rectus sheath, then inject 15-20 ml LA. Hydrodissection separates the rectus abdominis muscle from the posterior rectus sheath.
Evidence and Clinical Applications
- Compared to placebo or local wound infiltration analgesia, the rectus sheath block results in lower pain scores with opioid-sparing effects in both children and adults receiving umbilical hernia repair.
- Effective pain control in surgeries involving midline incisions.
- Can be combined with the TAP block for broader pain relief in anterior abdominal wall surgeries.
- Potential complications include peritoneal or bowel perforation, hematoma, and local systemic toxicity.
Ilioinguinal and Iliohypogastric Blocks
Clinical Background and Anatomy
- The ilioinguinal and iliohypogastric nerves originate from the L1 spinal nerve, emerge from the outer border of the upper part of the psoas major muscle, and cross the quadratus lumborum (QL) muscle.
- They penetrate the transversus abdominis muscle near the anterior iliac crest and communicate with each other between the transversus abdominis and the internal oblique muscle.
- Blocking these nerves with LA anesthetizes the inguinal wall, upper thigh, and suprapubic areas, similar to the TAP block.
Ultrasound-Guided Iliohypogastric Nerve Block Techniques
- Patient Position: Supine.
- Ultrasound Probe: High-frequency linear probe.
- Probe Position: Held at an oblique angle, moved from the anterior superior iliac spine (ASIS) to the umbilicus.
- Procedure: Identify the three abdominal muscle layers and deposit 10-20 ml LA in the fascia layer between the internal oblique and transversus abdominis muscles. Perform the block close and proximal to the ASIS before the nerve branches.
Evidence and Clinical Applications
- Indicated for surgeries in the inguinal and suprapubic areas.
- Effective perioperative pain control for inguinal hernia repairs in children and adults.
- Bilateral blocks reduce opioid consumption after cesarean sections and other lower abdomen gynecological surgeries.
- Potential complications include intraperitoneal injection and bowel injuries.
Quadratus Lumborum Block
Evidence and Clinical Applications
- Provides analgesia for abdominal surgeries.
- Lateral and posterior QL blocks offer more extensive analgesia than posterior TAP blocks, covering from T6-7 to L1.
- Anterior QL blocks provide analgesia for lower extremities and surgeries involving the hip and thigh, covering from T10 to L3.
- Superior to posterior TAP blocks in reducing postoperative pain and opioid consumption in cesarean section patients.
- Potential complications include peritoneal penetration, organ injuries, kidney damage, and local systemic toxicity due to the large volume of LA required for bilateral blocks.
- Further randomized controlled studies are needed to determine the optimal applications and differences between the lateral, posterior QL blocks, and the posterior TAP block.
Erector Spinae Plane Block
Clinical Background and Anatomy
- Drug spread anterior and inferior to the erector spinae muscle (ESM) fascial sheath resembles drug infiltration during paravertebral block (PVB).
- Drug spread outward and posterior to the ESM fascial sheath resembles drug infiltration during QL or posterior TAP block.
- Requires less technical expertise compared to other truncal blocks and is easier to perform than neuraxial, nerve plexus, and targeted nerve blocks.
- Likely to have fewer serious side effects (e.g., spinal cord damage, nerve trauma, pneumothorax).
- Continuous block can be administered by inserting a catheter, although further research is needed to evaluate the efficacy of single regional techniques.
Ultrasound-Guided ESP Block Techniques
- Patient Position: Sitting; lateral position may also be suitable.
- Ultrasound Probe: High-frequency linear probe.
- Probe Position: Parasagittal plane; similar scanning technique to thoracic PVB.
- Procedure: Identify the target transverse process (T5 for thoracic and upper abdominal procedures; T7 for lower abdominal procedures). Insert the needle in-plane from cranial to caudal direction until contacting the transverse process. Inject <1 ml fluid to separate the ESM from the transverse process, confirming the correct location. Inject 20-30 ml LA in the fascial plane beneath the ESM.
Evidence and Clinical Applications
- Various applications described, mostly in case reports and case series.
- Believed to provide analgesia similar to PVB, but with a much lower risk of side effects.
- Suitable for treating acute chest and abdominal pain following surgery.
- Particularly beneficial for higher-risk patients, such as those with coagulation disorders.
- Prospective studies are needed to confirm its efficacy, safety, and clinical applications.
Chest Wall Blocks
PECS
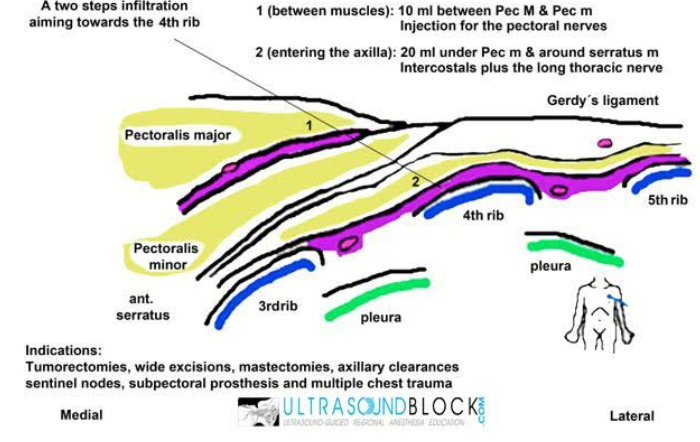
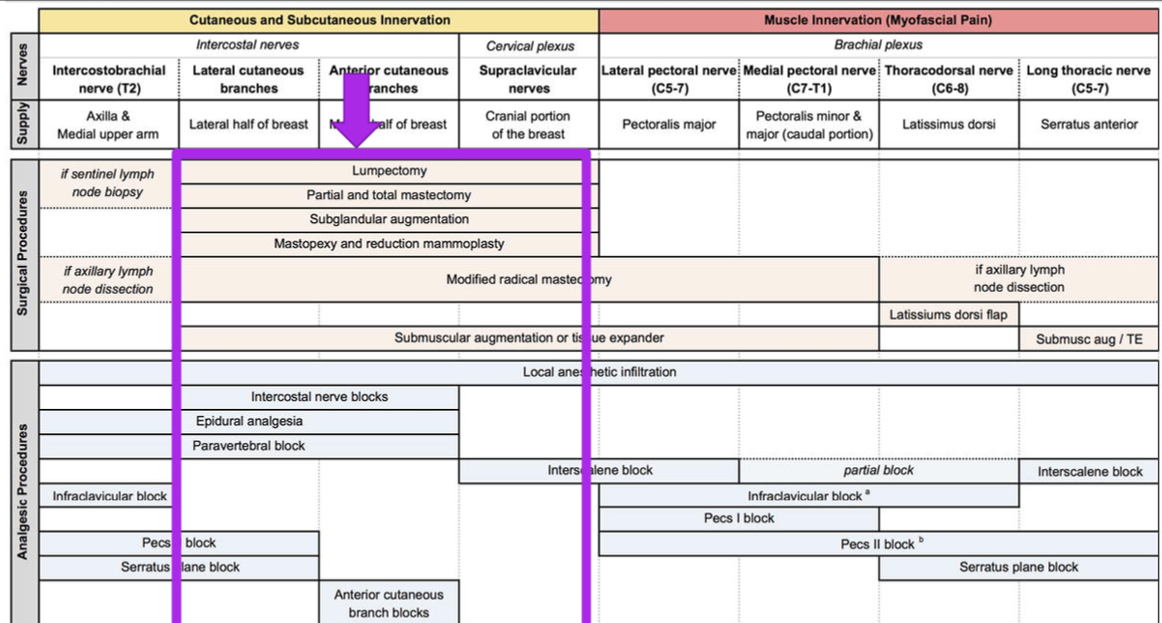
Paravertebral Block Vs PEC
Paravertebral
- Complications: Pneumothorax, high uptake – LAST, epidural spread, sympathectomy, vagal response, technically challenging, anticoagulation, requires prone or sitting position.
PECs II
- Advantages: Technically easy to perform, provides cutaneous and myofascial coverage, high volume block – LAST, disrupts tissue planes, lacks coverage for medial breast, suitable for supine position.
PEC 1
- Target Nerves: Lateral and medial pectoral nerves
- Provides: Myofascial analgesia
- Indications: Breast expanders, radical mastectomy/reconstructive surgery
- Limitations: Does not cover medial chest and axilla
PEC-2
- Targets: T2-4 intercostal branches, thoracodorsal, long thoracic → lateral breast and axillary coverage
- Spares: Medial chest (anterior cutaneous branches)
- Caution: Axillary dissection (LTN)
Serratus Anterior Block (SAP Block)
Clinical Background and Anatomy
- Patient Position: Sitting or lateral.
- Ultrasound Probe: High-frequency linear probe.
- Procedure:
- Scan beneath the clavicle to identify the second rib.
- Move the probe laterally and caudally toward the mid-axillary line, counting the ribs.
- Identify the fourth and fifth ribs and the serratus anterior and latissimus dorsi muscles.
- Inject 20 ml of LA solution either superficial to the serratus anterior (between the latissimus dorsi and the serratus anterior) or deep between the serratus anterior and external intercostal muscles.
Evidence and Clinical Applications
- Initially developed for analgesia after breast surgery.
- Indicated for perioperative pain relief in surgeries involving the anterior chest wall and the axilla (Pecs 2) or the posterolateral chest wall (serratus anterior block).
- Does not anesthetize the anterior cutaneous branches of the intercostal nerves; the medial aspect of the breast, including the nipple and areola, are not blocked.
- To block the anterior cutaneous branches, the pectointercostal and transversus thoracic muscle plane blocks have been described.
- Recent studies have shown the efficacy of pectoral plane blocks, which are associated with lower pain scores and opioid-sparing effects compared to placebo.
- Comparing Pecs blocks with single thoracic paravertebral injections has produced conflicting efficacy results.
- Potential complications include pneumothorax and injury to the thoracodorsal artery. Data on complications are limited due to the novel nature of these techniques.
Paravertebral Block (PVB)
Clinical Background and Anatomy
- Thoracic Paravertebral Space:
- Contains thoracic spinal nerves, thoracic sympathetic chain, ramus communicans, intercostal vessels, and fat tissue.
- Communicates laterally with intercostal spaces and medially with the epidural space through the intervertebral foramen.
- Triangular in transverse section: medial base (vertebral body, articular process, intervertebral foramen), anterolateral border (parietal pleura), posterior border (transverse process, heads of ribs, superior costotransverse ligament).
- Block Mechanism:
- Depositing LA induces blockade of ipsilateral somatosensory and sympathetic nerves.
- Single injected bolus of LA can reach several adjacent dermatomes due to continuous communication within the space, although the spread level varies.
Ultrasound-Guided Thoracic PVB Techniques
- General Landmarks: Transverse process, rib, and pleura.
Transverse Approach
- Ultrasound Probe Position: Transversely to obtain an axial view of the trunk lateral to the midline.
- Procedure:
- Use a high-frequency linear probe to obtain an image of the bony structures at the target vertebral level.
- Move the probe slightly cephalad until the rib disappears, showing the transverse process and pleura.
- Insert the needle laterally to medially, ensuring the tip enters the paravertebral space under the transverse process and above the pleura.
- Inject 10-20 ml LA, with an option to insert a continuous catheter if required.
- Reported blockade: approximately five dermatomes with an average of 10 ml LA; some studies indicate four to six dermatomes with 20 ml LA.
- Single injection duration: 3-4 hours for lidocaine, 8-12 hours for ropivacaine or bupivacaine.
Parasagittal Approach
- Ultrasound Probe Position: Vertical plane lateral to the spinous process.
- Procedure:
- Identify the ribs and pleura corresponding to the dermatomes.
- Move the probe medially to locate the transverse process.
- Insert the needle in a caudal to cephalad trajectory.
- Penetrate the superior costotransverse ligament with a “pop” sound or loss of resistance.
- Use a Tuohy needle due to the steep angle and to avoid pleural damage.
- Lower risk for unintended epidural injection and catheter migration compared to the transverse approach.
Evidence and Clinical Applications
- Indications:
- Provides perioperative pain relief for various abdominal surgeries (e.g., renal surgeries, herniorrhaphies, cholecystectomies) involving thoracic spinal nerve dermatomes.
- Effective for pain relief after breast surgeries, thoracic surgeries, and chest wall surgeries.
- Comparative Efficacy:
- Superior pain relief and reduced opioid requirement compared to intercostal nerve block, intrapleural analgesia, and intrathecal opioids.
- Equivalent or superior analgesic efficacy compared to thoracic epidural analgesia (TEA) with a better side effect profile and higher success rate.
- Effective in controlling acute pain with reduced risk of complications.
- Optimal LA and adjuvant doses for single injection and continuous analgesia are not yet established.
- Potential Complications:
- Pneumothorax, hematoma, neurological injury, unintended intrathecal or epidural injection, LA toxicity.
- Further studies are needed to determine optimal catheter placement for continuous paravertebral analgesia.
Links
- Upper limb blocks
- Lower limb blocks
- Ortho regionals
- Anticoagulation and blocks
- Labour analgesia
- Analgesia in ICU
- Thoracic surgery analgesia
Past Exam Questions
Pectoral Blocks (PEC) for Hemithorax Analgesia
Pectoral blocks (PEC) are an alternative to thoracic epidural or paravertebral blocks to provide analgesia and anaesthesia to the hemithorax.
a) What are the indications for a PEC 1 block? (3)
b) How does the Modified PEC’s 2 block differ from the PEC’s 1 block? (2)
c) What are the indications for a Modified PEC’s 2 block? (2)
d) What are the advantages and disadvantages of continuous peripheral nerve blocks? (3)
References:
- FRCA Mind Maps. (2024). Retrieved June 5, 2024, from https://www.frcamindmaps.org/
- Koh, W. U. and Lee, J. H. (2018). Ultrasound-guided truncal blocks for perioperative analgesia. Anesthesia and Pain Medicine, 13(2), 128-142. https://doi.org/10.17085/apm.2018.13.2.128
- Wai, C. L. W. and Irwin, M. G. (2012). Regional blocks in orthopaedics. Anaesthesia &Amp; Intensive Care Medicine, 13(3), 89-93. https://doi.org/10.1016/j.mpaic.2011.12.004
- Horlocker, T. T., Vandermeuelen, E., Kopp, S. L., Gogarten, W., Leffert, L., & Benzon, H. T. (2019). Regional anesthesia in the patient receiving antithrombotic or thrombolytic therapy: american society of regional anesthesia and pain medicine evidence-based guidelines (fourth edition). Obstetric Anesthesia Digest, 39(1), 28-29. https://doi.org/10.1097/01.aoa.0000552901.03545.fb
- Checketts, M. R. (2016). Intravenous regional anaesthesia. Anaesthesia &Amp; Intensive Care Medicine, 17(4), 192-193. https://doi.org/10.1016/j.mpaic.2015.12.013
- Ahmed A, et al. Continuous paravertebral block versus epidural for thoracotomy: randomised trial. JAMA Surg 2025.
- Lim J, et al. Meta-analysis of erector spinae plane block for VATS. Anesth Analg 2024.
- Chen X, et al. Pectoral, serratus and paravertebral blocks for breast cancer surgery: network meta-analysis. Pain Pract 2024.
- Lee S, et al. ESPB vs SAPB after mastectomy: systematic review and meta-analysis. J Anesth Crit Care 2024.
- Kaya V, et al. Quadratus lumborum vs ESPB vs intrathecal morphine for Caesarean: RCT. Anaesthesia 2023.
- O’Connor H, et al. TAP block effectiveness for laparoscopic gynaecology: systematic review. Br J Anaesth 2024.
- Patel N, et al. Bilateral oblique sub-costal TAP catheters for robotic prostatectomy: systematic review. Surg Endosc 2025.
- Zhang Y, et al. Ultrasound-guided rectus sheath block in umbilical hernia repair: RCT. Pain Physician 2024.
- Johnson M, et al. Analgesic profile of PEC II plus serratus anterior blocks versus TPVB in radical mastectomy. Reg Anesth Pain Med 2024.
- Smith D, et al. Rectus sheath block for open umbilical hernia with cirrhosis. Pain Physician 2023.
- FRCA Mind Maps. (2024). Retrieved June 5, 2024, from https://www.frcamindmaps.org/
- Anesthesia Considerations. (2024). Retrieved June 5, 2024, from https://www.anesthesiaconsiderations.com/
- Boutique Workshops. (n.d.). In NYSORA. Retrieved June 26, 2024, from https://www.nysora.com/mec-category/boutique-workshops/
- ASRA Pain Medicine. (n.d.). Guidelines. Retrieved June 27, 2024, from https://www.asra.com/guidelines-articles/guidelines
- European Society of Regional Anaesthesia & Pain Therapy (ESRA). (n.d.). Guidelines. Retrieved June 27, 2024, from https://esraeurope.org/guidelines/
- Teaching videos
Summaries:
Paravertebral blocks
Anterior abdominal wall nerve blocks
Copyright
© 2025 Francois Uys. All Rights Reserved.
id: “82303bc8-5d83-431a-83ac-ec78bfe5376b”



