- Summary of Approach to Patient with Pacemaker or ICD
- Essentials
- Peri-operative Considerations
- Preoperative Considerations
- Routine Investigations
- Intraoperative Considerations
- Postoperative Management
- Pacemaker and ICD
- 1. Aetiology for Pacemaker Insertion
- 2. Type of Pacemaker and Pacing Mode
- 3. Pacemaker Dependence – How to Assess
- 4. Device Interrogation – Who Needs It and When
- 5. Pacemaker Programming Strategy: ‘On’ (Asynchronous) Vs ‘Off’ (Inhibitory)
- 6. R-on-T Phenomenon
- 7. Switching Off an ICD
- 8. Defibrillation in Pacemaker Patients – Safe Approach
- 9. Intraoperative Indications for Defibrillator Pad Placement
- 10. Special Considerations: Leadless PMs and Subcutaneous ICDs
- 11. Identifying Pacemaker Dependence
- 12. Preoperative Investigations
- 13. Magnet Use
- 14. Intraoperative Monitoring
- 15. Electrical Interference (EMI) – Sources and Management
{}
Summary of Approach to Patient with Pacemaker or ICD
Recommendations for Management of Cardiac Implantable Electronic Devices
| Procedure | Intra-operative Pacemaker Monitoring | Pacemaker Reprogramming | Postoperative Pacemaker Check | Implantable Cardioverter-Defibrillator Deactivation/Re-activation |
|---|---|---|---|---|
| Surgery below umbilicus or upper limb distal to elbow | + | − | − | + |
| Surgery above umbilicus or upper limb proximal to elbow | + | ±a | + | + |
| Cardiac surgery | + | ±a | + | + |
| Ophthalmic surgery (if unipolar diathermy anticipated) | + | ±a | ±a | + |
| Endoscopy procedure | ±a | − | − | ±c |
| Dental surgery (only if diathermy use is anticipated) | ±a | ±b | ±b | ±c |
| Lithotripsy | + | ±b | ±b | ±c |
| Electroconvulsive therapy | + | ±b | ±b | ±c |
| Nerve conduction studies | + | ±a | ±a | − |
Notes
- a: Consider reprogramming if patient is pacemaker dependent; postoperative pacemaker check required if reprogrammed.
- b: Consider reprogramming if patient is pacemaker dependent; interrogate pacemaker within 1 month after procedure.
- c: Deactivate implantable cardioverter-defibrillators peri-operatively and reactivate postoperatively; carry out checks after procedure.
Essentials
Classification
- Temporary: Transcutaneous / Epicardial / Transvenous
- Permanent: Placement of ≥ 1 electrode(s) in ≥ 1 chamber(s)
- Pacing: Single Chamber / Dual chamber / Rate Responsive
Rate Modulation
- Pacemaker senses patient activity and adjusts the pacing rate to meet metabolic requirements
- Rate is increased in response to (i) Motion detected by an accelerometer and/or (ii) Minute Ventilation detected by Thoracic Impedance
- Anaesthesia: Sensors will adjust rate acc to ventilation and/or motion or interference – so RM must be disabled
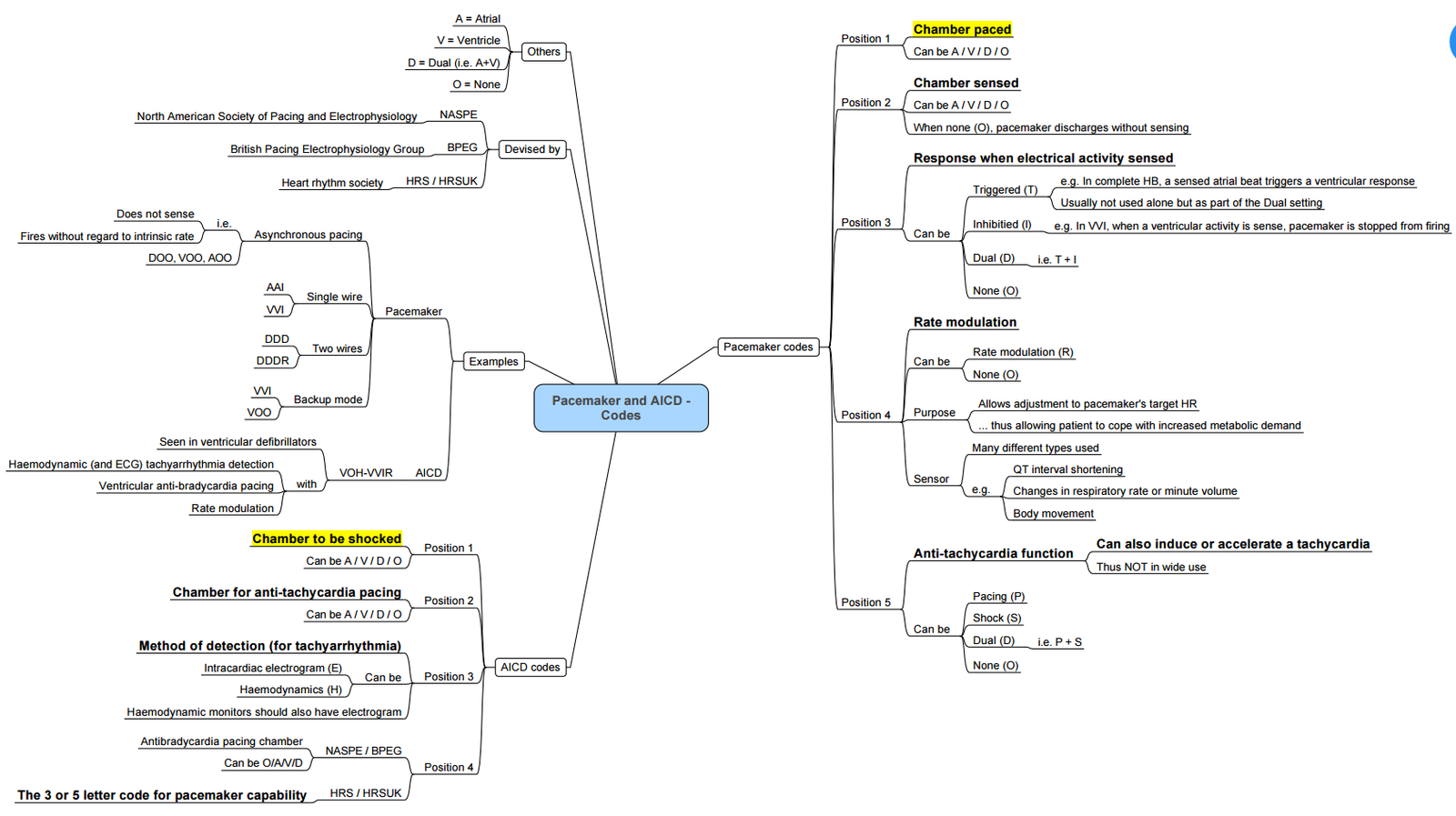
Pacemaker Code System
| I | II | III | IV | V |
|---|---|---|---|---|
| Chamber Paced | Chamber Sensed | Response to Sensing | Rate Responsiveness | Multisite Pacing |
| 0 = none | 0 = none | 0 = none | 0 = none | 0 = none |
| A = atrium | A = atrium | T = triggered | R = rate modulation | A = atrium |
| V = ventricle | V = ventricle | I = inhibited | V = ventricle | |
| D = dual (A+V) | D = dual (A+V) | D = dual (T+I) | D = dual (A+V) | |
| S = single (A or V) | S = single (A or V) |
- DDD (synchronous): Ensures coordination between atria and ventricles if one or both are initiating an impulse.
- Four rhythms possible: 1. NSR 2. Atrial sensed, ventricle paced 3. Atrial paced, ventricle sensed 4. Atrial and ventricular pacing
- Ensures that atrial events are followed by ventricular contraction, but inhibits itself if a native QRS is detected. Also ensures that an atrial contraction occurs, thus its advantage over VDD is that it guarantees atrial kick.
Generic Defibrillator Code (NBD): NASPE/BPEG
| Position I | Position II | Position III | Position IV |
|---|---|---|---|
| Shock Chamber(s) | Antitachycardia Pacing Chamber(s) | Tachycardia Detection | Antibradycardia Pacing Chamber(s) |
| O = None | O = None | E = Electrogram | O = None |
| A = Atrium | A = Atrium | H = Hemodynamic | A = Atrium |
| V = Ventricle | V = Ventricle | V = Ventricle | |
| D = Dual (A+V) | D = Dual (A+V) | D = Dual (A+V) |
Position IV is expanded to the full pacemaker coding e.g. VVE-DDDRV
Absolute Indications for Pacemaker
- Sick sinus syndrome
- Symptomatic sinus bradycardia
- Tachycardia-bradycardia syndrome
- Atrial fibrillation with sinus node dysfunction
- Complete atrioventricular block (third-degree block)
- Chronotropic incompetence
- Prolonged QT syndrome
- Cardiac resynchronization therapy with biventricular pacing
Unipolar Vs Bipolar Diathermy
- Bipolar: Greater risk for electromagnetic interference (the box makes up part of the circuit).
- Unipolar: Current runs from the tip and back to the tip of the lead (less risk of electromagnetic interference).
Rough Guideline to the Choice of Pacing Mode
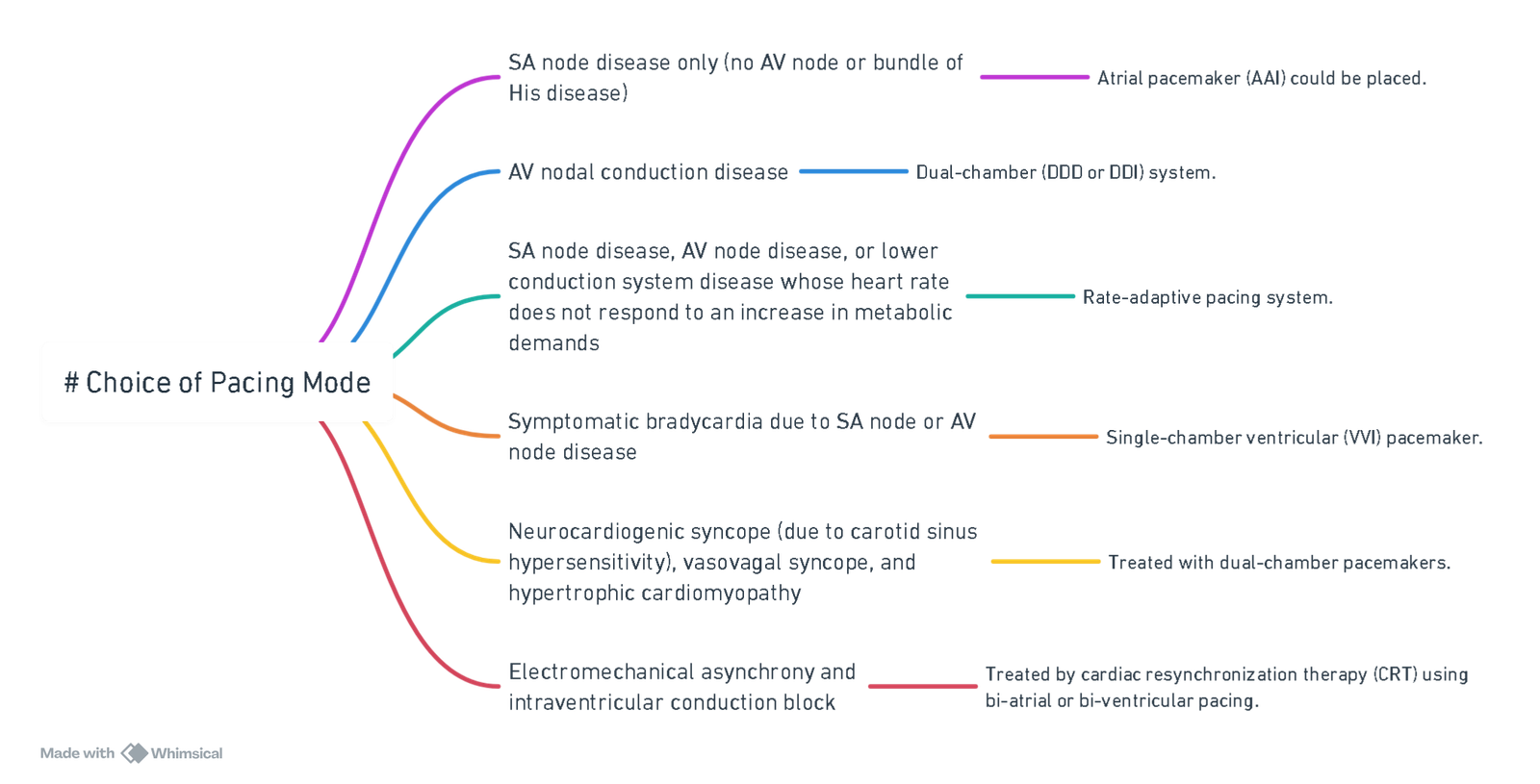
View or edit this diagram in Whimsical.
Rate Responsive Pacemaker
- Definition: Rate responsiveness.
- Benefit: The ability to increase heart rate in response to motion or sensed physiological exertion.
- Anaesthesia Considerations: Excessive pacing rates may be triggered by increased respiratory rate, increased tidal volume, electrocautery, and patient movement.
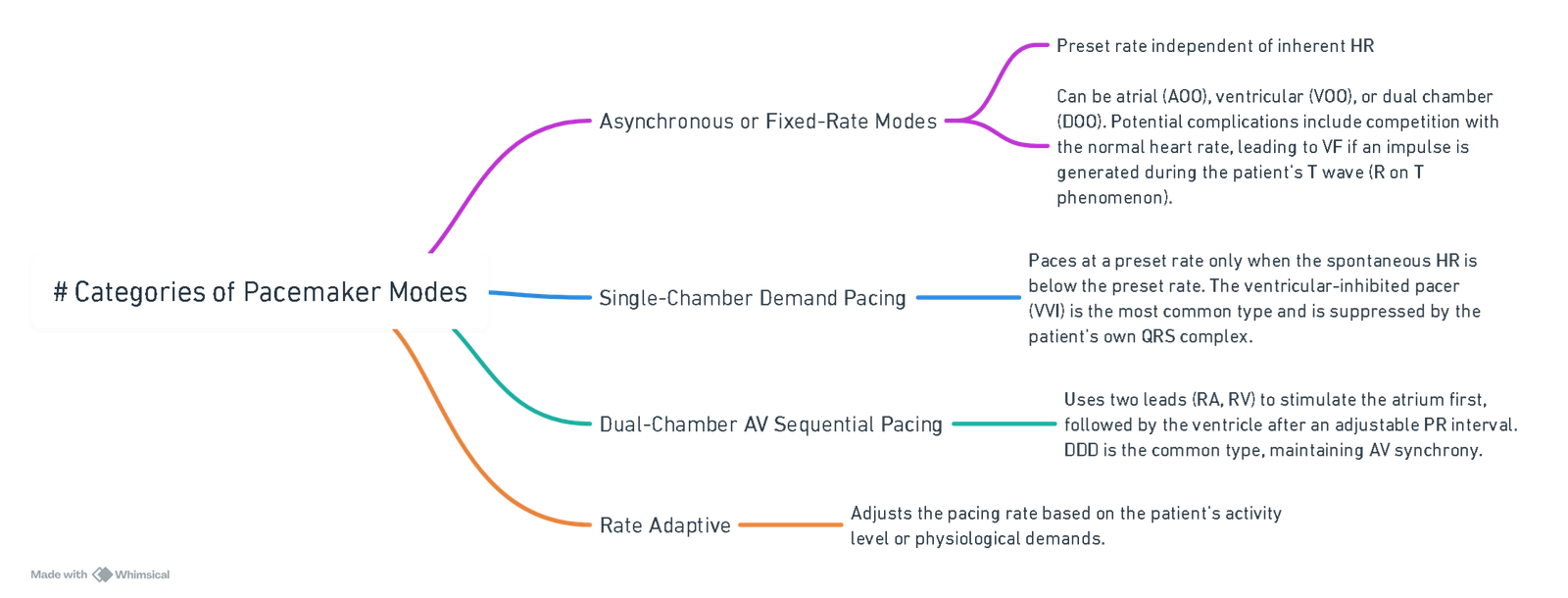
View or edit this diagram in Whimsical.
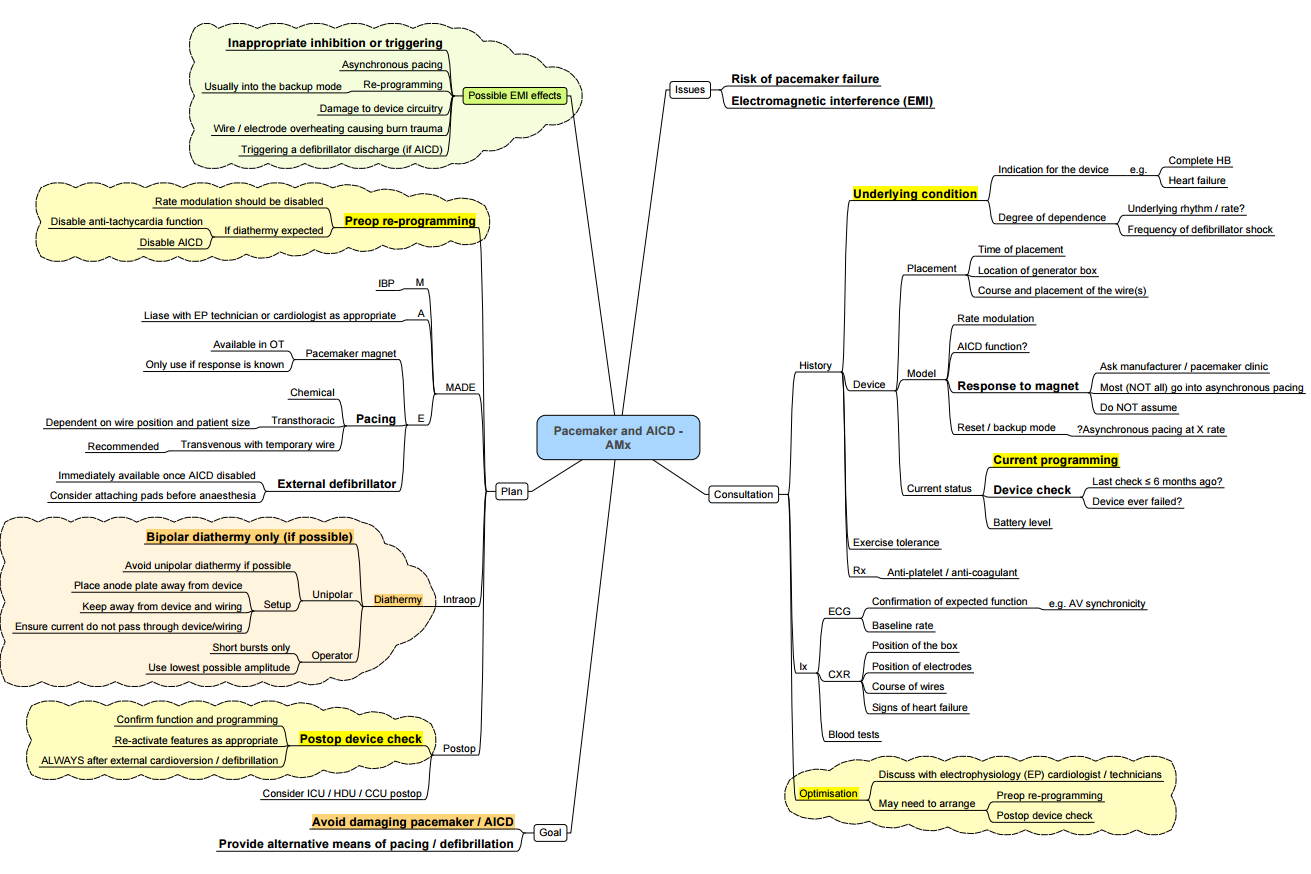
Peri-operative Considerations
Pacemaker
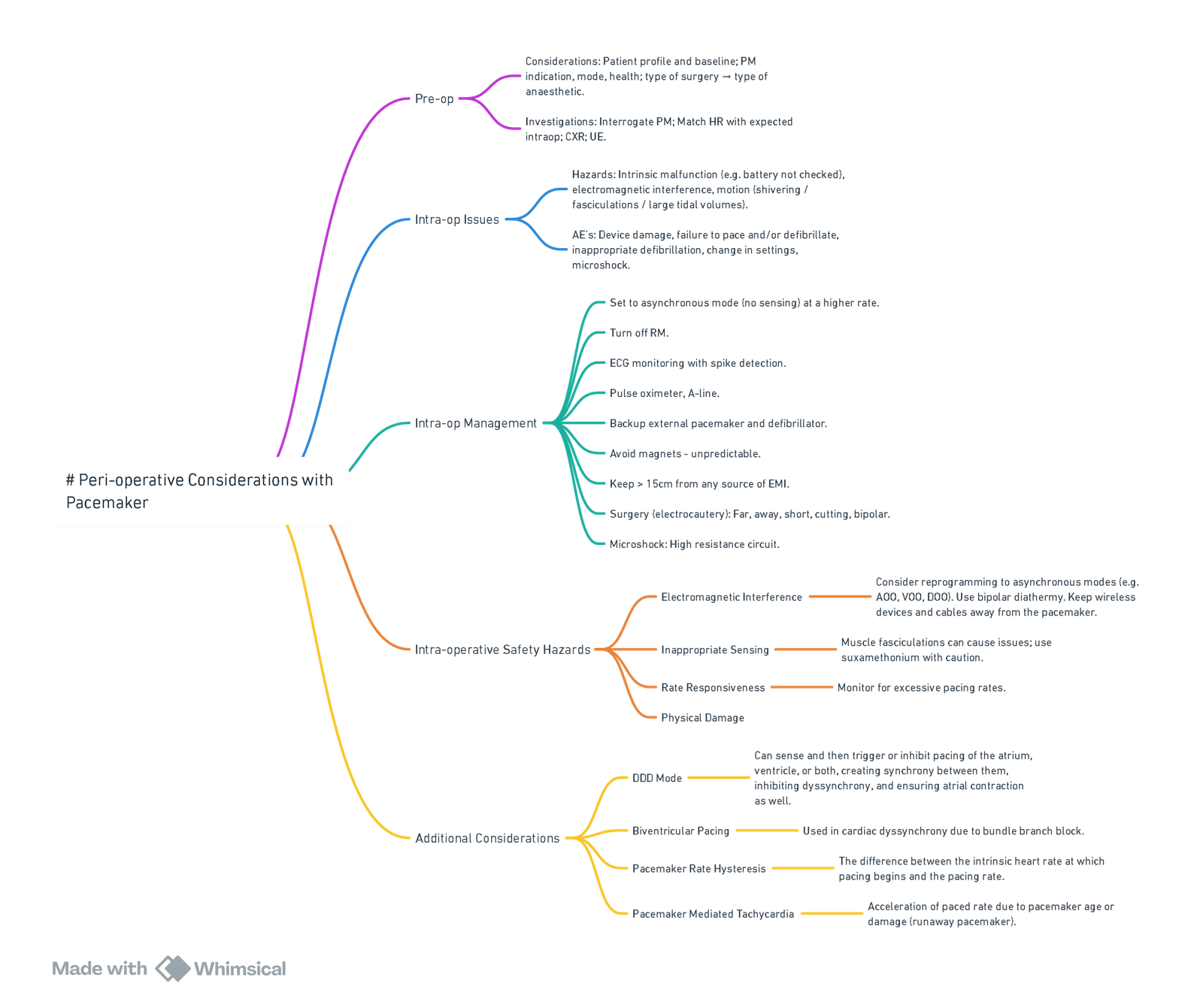
View or edit this diagram in Whimsical.
Preoperative Considerations
- Check patient notes:
- Indication for insertion
- Date of insertion
- Most recent device checks
- Note the mode of action of the PPM
- If rate-modulating (rate-responsive), deactivate prior to anaesthesia
- Switch to bipolar mode (less prone to interference)
Routine Investigations
- ECG:
- Look for signs of capture
- Assess underlying rhythms
- Check for lead fracture
- CXR:
- Confirm position of pacing box
- Assess for evidence of congestive cardiac failure (CCF)
- Electrolytes:
- Correct abnormalities (can cause loss of capture)
- Routine investigations not always required, but consider based on clinical context
Intraoperative Considerations
- Anaesthetic technique:
- Avoid suxamethonium (sux) if possible—fasciculations may disrupt capture
- Ensure U&Es are normal
- Limit monopolar diathermy use
- If used, place return plate distant from the pacemaker
- Contingency plan for pacing failure:
- Percussive pacing
- Isoprenaline infusion
- External pacing (typically set at 80 mA)
- Transvenous or transoesophageal pacing (longer to set up)
- Magnets:
- Should not be used during surgery to manage pacing
Postoperative Management
- Ensure PPM function is checked post-operatively
ICD (Implantable Cardioverter Defibrillator)
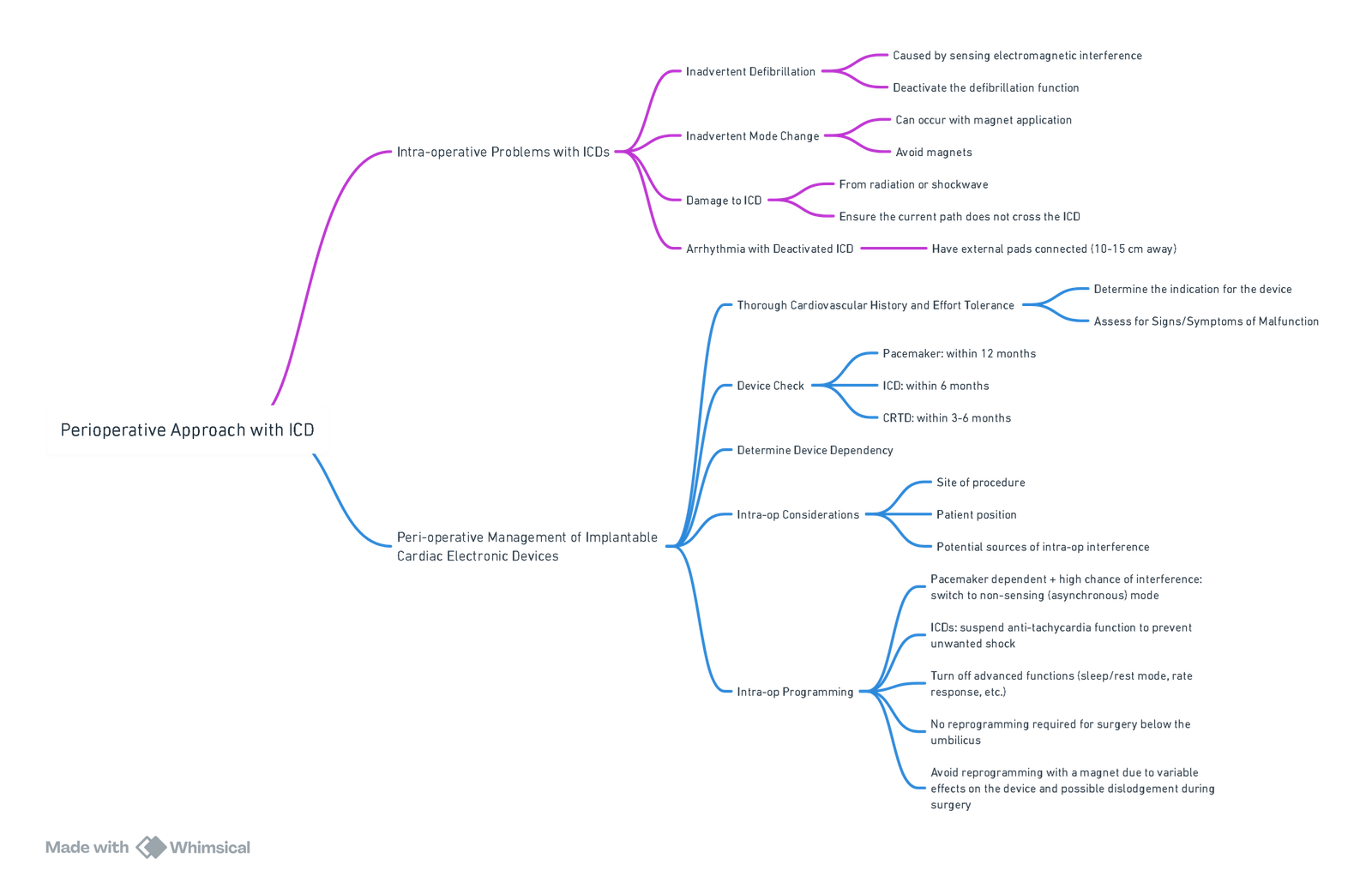
View or edit this diagram in Whimsical.
Pacemaker and ICD
Pacemaker
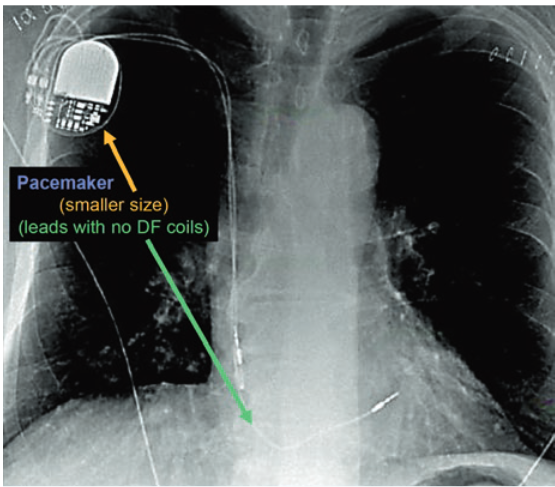
Radiographic ID
- Smaller generator
- Discreet right ventricular lead (stable diameter)
- With or without right atrial lead or coronary sinus lead
Indications
- Patients with symptomatic sinus node dysfunction and bradycardia
- Patients with complete AV block (symptoms less relevant)
- Hypersensitive carotid sinus syndrome and neurocardiogenic syncope
Effect of Magnet
- Suspends sensing of intrinsic rhythm.
- Pacing in an asynchronous mode: the rate depends on the manufacturer and the battery life; if the battery life is low, the rate may not be adequate for surgery.
- Turns off “rate response.”
Other Effects
Electrocautery
- Faulty sensing of intrinsic activity causing inappropriate inhibition of pacemaker activity
- More prominent with monopolar cautery
- More likely with above-the-waist surgery
- Possible device reset or damage to the generator, or the leads, but unlikely
Radiation Therapy
- Possible device reset when performed near the device
Radiofrequency
- Electrocautery-like electromagnetic interference that could cause inappropriate inhibition of pacemaker activity, which is more likely with procedures above the waist
- Possible device reset or damage to the generator, or the leads, but unlikely
ICD
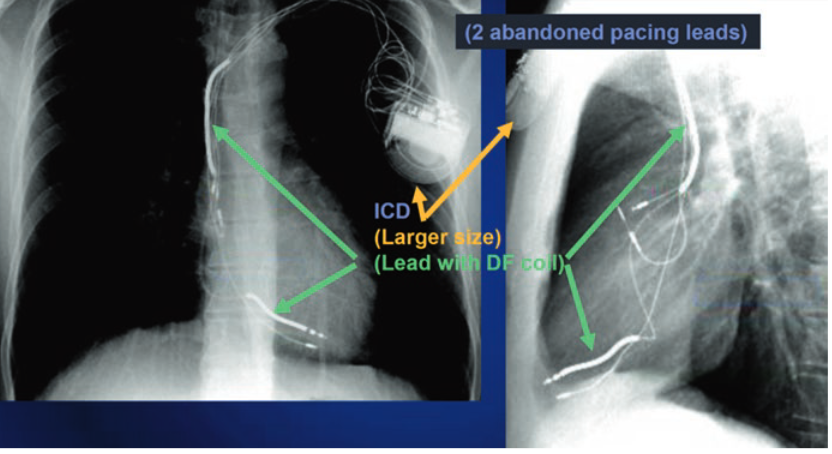
Radiographic ID
- Larger generator
- Prominent right ventricular lead, also known as shock coils. They appear as two metallic segments along the length of the ICD lead.
Indications
- Patients at risk of sudden cardiac death: Prior ventricular tachycardia or fibrillation, low ejection fraction
- Long QT syndrome
- Hypertrophic cardiomyopathy
- Arrhythmogenic right ventricular dysplasia
- Cardiac transplantation
- Primary electrical disease: idiopathic ventricular fibrillation, short QT syndrome, Brugada syndrome, and catecholaminergic polymorphic ventricular tachycardia
Anesthesia for Brugada Syndrome
- Requires ICD
- Intraoperative considerations:
- Turn off ICD; use ECG monitoring and pacing pads
- Monitor electrolytes and maintain normal levels
- Maintain normothermia
- Avoid or cautiously perform vagotonic procedures (e.g., pneumoperitoneum)
- Avoid propofol infusions (bolus can be used), local anesthetics, and alpha-2 agonists. Ketamine and etomidate may also increase ST segment elevation.
- Monitor for at least 36 hours in a high-care unit.
- Monitor for VT/VF intraoperatively: If it occurs:
- Perform defibrillation
- Administer isoprenaline infusion if an arrhythmogenic storm occurs (>2 episodes of VT/VF in 24 hours)
- Check electrolytes and address reversible causes
- Quinidine can also be used orally
- Remove triggering drugs
Effects of Magnet
- Varies depending on device, manufacturer, and programming.
- Generally turns off detection of tachycardia and tachycardia therapy (discharge and pacing).
- Typically has no effect on the pacemaker (pacing will not become asynchronous).
- For pacemaker-dependent patients, it is best to reprogram the device to address both tachycardia and bradycardia therapy due to the risk of electrical interference and pacemaker malfunction.
Other Effects
Electrocautery
- Faulty sensing of intrinsic activity causing inappropriate sensing of arrhythmias
- More prominent with monopolar cautery
- Possible device reset or damage to the generator or leads, but unlikely
Radiation Therapy
- Possible device reset when performed near the device
Radiofrequency
- Electrocautery-like electromagnetic interference that could cause inappropriate arrhythmia sensing inhibition
- Possible device reset or damage to the generator or leads, but unlikely
The Radiographic Image of a BiV ICD
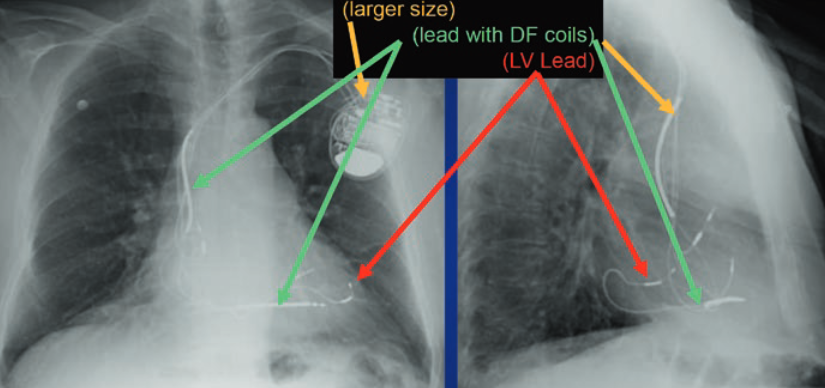
Radiographic ID
- Larger generator
- Prominent right ventricular lead (shock coils)
- Right atrium lead
- Coronary sinus lead
Indications
- Treatment of left ventricular dysfunction and heart failure with prolonged ventricular conduction and heart failure symptoms.
- Required ventricular pacing and low ejection fraction (EF):
- Right ventricular (RV) pacing in patients with low EF increases CHF admissions and mortality.
- Cardiac resynchronization therapy:
- Improves exercise tolerance and mortality.
- Continuous pacing provides better hemodynamic stability.
Why Would a Patient Become Pulseless with a Magnet?
- Most likely, the patient has a BiV ICD and low EF and is pacemaker-dependent.
- The device functioned appropriately with the magnet, which suspended tachyarrhythmia detection.
- Pacing was inhibited by the prolonged use of electrocautery.
- Pacing returns to an unresponsive myocardium after a prolonged period of asystole, which might have led to PEA arrest.
Cardiac Resynchronisation Therapy (CRT) Devices
Overview
- CRT devices are cardiac implantable electronic devices (CIEDs).
- Indicated for heart failure with poor left ventricular (LV) function and left bundle branch block (LBBB).
Device Configuration
- Consists of three leads:
- Atrial lead
- Right ventricular (RV) lead
- Left ventricular (LV) lead placed in the coronary sinus, as laterally as possible
- Aims to synchronously pace both RV and LV following detection of the atrial beat.
- CRT devices need to be checked within three months of insertion (battery drains faster)
Mechanism of Action
- Device senses the atrial signal.
- Delivers simultaneous pacing to the right and left ventricles.
- Goal: Restore synchronous ventricular contraction.
Clinical Benefits
- Improves left ventricular ejection fraction (LVEF) by approximately 15%.
Device Variants
- CRT-P: Includes pacemaker (PM) functionality only.
- CRT-D: Includes both pacemaker and implantable cardioverter-defibrillator (ICD) functions.
Cardiothoracic Anaesthetic Society of South Africa (CASSA Statements and Algorithms 2021)
1. Preoperative Device Interrogation
- Standard of care for all CIEDs
- Ideally scheduled during the week prior to surgery
- If technologist not available, may proceed if:
- PM checked within 12 months
- ICD checked within 6 months
- CRT (P or D) checked within 3 months
If Device Reprogramming is Required
- Should occur on the morning of surgery
- Revert to baseline as soon as ESU is no longer needed
- Monitor patient in a high dependency unit (HDU)
2. Preoperative Device Evaluation (if Technologist is available)
-
Identify:
- Device type: PM / ICD / CRT-P / CRT-D
- Manufacturer and model
- Indication and date of insertion
- Pacemaker dependency
- Battery status: BOL / EOL / RRT → replace preoperatively if RRT
- Pacing thresholds, especially for new leads
- Any rejection activity
- Magnet response (and removal)
- Reset rate if operation scope may interfere
- Device or lead alert / recall status
3. Preoperative Strategy (if Technologist Unavailable in emergency)
- Review:
- CXR
- ECG to assess dependency
- Patient device card
- Contact cardiologist
- Use manufacturer 24-hour helpline*
- Confirm last device interrogation:
- PM < 12 months
- ICD < 6 months
- CRT (P or D) < 3 months
- Magnet testing:
- May apply magnet preoperatively to assess PM rate or ICD tone
- Blind magnet application not recommended unless emergency
4. Magnet Use – General Principles
- Not recommended intraoperatively by ASA
- Permitted by Canadian and European guidelines
- Pre-op interrogation should assess magnet response
Magnet Effects by Device
| Device Type | Response to Magnet |
|---|---|
| PM | 85 bpm (65 bpm if RRT), switches to DOO/VOO/AOO, disables rate responsiveness |
| ICD | Suspends anti-tachy therapy & ATP, no effect on pacing, emits 10s tone |
| CRT-P | Behaves like pacemaker: DOO at 85 bpm (65 bpm if RRT) |
| CRT-D | Suspends shocks & ATP, no pacing effect |
| Leadless PM | Depends on manufacturer:- Medtronic: no effectSt. Jude: switches to VOO |
5. Use of PM-on Vs ICD-on Protocols
PM-on Protocol
- Use magnet intraoperatively to switch PM to asynchronous mode (DOO)
- Reasonable if:
- Surgical site > 15 cm from generator/leads
- OR surgery below umbilicus/iliac crest
- AND dispersive pad distal to surgical site
ICD-on Protocol
- Use magnet to suspend anti-tachy therapy
- Reasonable if:
- Surgical site > 15 cm from generator/leads
- OR surgery below umbilicus/iliac crest
- AND dispersive pad distal to surgical site
CASSA Approaches
Pacemaker or CRT-P Patient
→ What is the Operation Site in relation to the Pacemaker?
- Greater than 15 cm from device AND diathermy dispersive electrode away from device
- Proceed without changes
- Greater than 15 cm from device AND <5s bursts of monopolar diathermy
- → Can a magnet be secured if needed?
- Yes:
- Proceed
- Apply magnet only if EMI causes asystole or oversensing
- Remove magnet post-op
- Re-interrogate device before discharge
- No (e.g., patient prone):
- Preoperatively reprogram to DOO/VOO/AOO
- Disable rate responsiveness
- Reprogram to baseline once diathermy use ends
- Yes:
- → Can a magnet be secured if needed?
- < 15 cm from device OR using Argon Beam / long monopolar bursts in PM-dependent patient
- Reprogram PM to DOO/VOO/AOO
- Disable rate responsiveness
- Restore original settings when electrosurgery complete
ICD or CRT-D Patient
→ What is the Operation Site in relation to the ICD
- Greater than 15 cm from generator or leads
- Proceed without changes
- < 15 cm AND using only harmonic scalpel or bipolar diathermy
- → Can a magnet be secured if needed?
- Yes:
- Proceed
- Apply magnet if EMI causes shocks/ATP
- Especially in eye/hand surgery
- Magnet does NOT affect pacing settings
- Re-interrogate ICD before discharge
- No (e.g., prone):
- Reprogram to DOO/VOO/AOO
- Disable anti-tachyarrhythmia therapy + rate responsiveness
- Reprogram when EDI is no longer used
- Yes:
- → Can a magnet be secured if needed?
- < 15 cm AND using Argon Beam or long monopolar bursts in PM-dependent patient
- Reprogram ICD:
- Mode: DOO/VOO/AOO
- Disable tachy therapy & rate responsiveness
- Restore original settings when electrosurgery is complete
- Reprogram ICD:
Notes
- Interrogate all devices preoperatively
- Always document magnet response
- Monitor in HDU if settings are changed
- Avoid blind magnet use unless emergency
- Place dispersive pad away from device
Perioperative Management of Pacemakers and ICDs VIVA
1. Aetiology for Pacemaker Insertion
- Symptomatic bradycardia
- Complete heart block (3rd-degree AV block)
- Sinus node dysfunction
- Atrial fibrillation with slow ventricular response
- Congenital conduction disease
- Post-cardiac surgery conduction abnormalities
- AV node ablation for rate control
2. Type of Pacemaker and Pacing Mode
Device Types
- Single-chamber (e.g., VVI, AAI)
- Dual-chamber (e.g., DDD)
- Cardiac Resynchronization Therapy (CRT-P)
NBG Code Overview
- Position I: Chamber paced (A = atrium, V = ventricle, D = dual)
- Position II: Chamber sensed
- Position III: Response to sensing (I = inhibited, T = triggered, D = dual)
- Position IV: Rate modulation (R = rate response)
- Position V: Antitachy therapy (applicable to ICDs)
3. Pacemaker Dependence – How to Assess
- No reliable intrinsic rhythm to maintain perfusion
- ECG: 100% pacing with no underlying rhythm
- Device interrogation confirms reliance
- Clinical history: asystole, syncope, AV node ablation
- Absence of escape rhythm
4. Device Interrogation – Who Needs It and When
- All CIEDs should be interrogated preoperatively
- ICD: within 6 months
- Pacemaker: within 12 months
- CRT: within 3–6 months
- Assess: function, battery, thresholds, magnet response
5. Pacemaker Programming Strategy: ‘On’ (Asynchronous) Vs ‘Off’ (Inhibitory)
Asynchronous (VOO/DOO)
- Avoids EMI inhibition
- Used in pacing-dependent patients
Inhibitory (VVI/DDI)
- Preserves AV synchrony
- Used if EMI unlikely and patient is not dependent
Pros and Cons
- Asynchronous: prevents inhibition; risk of R-on-T and loss of synchrony
- Inhibitory: maintains synchrony; vulnerable to EMI
6. R-on-T Phenomenon
- Occurs when R wave/pacing spike falls on T wave (relative refractory period)
- Heterogeneous ventricular conduction → risk of re-entry
- May trigger polymorphic VT or VF
- Phase 3 (K⁺ efflux) of ventricular action potential
- Risk factors: long QT, bradycardia, ischaemia
- Triggered by asynchronous pacing, EMI, inappropriate shocks
- Prevention: confirm pacing dependence before asynchronous pacing, monitor QT, correct electrolytes
7. Switching Off an ICD
- Prevents inappropriate shocks from EMI
- Preferred: use programmer
- Alternative: magnet (suspends shock only, doesn’t affect pacing)
- Must be done in a monitored setting
- ECG, perfusion monitoring, defib pads applied
Risks
- Loss of VT/VF protection
- Especially critical in secondary prevention ICDs
8. Defibrillation in Pacemaker Patients – Safe Approach
- Yes, defibrillate when indicated (e.g., VF, pulseless VT)
Precautions
- Avoid placing pads over the device
- Keep pads ≥15 cm from generator
- Prefer anteroposterior pad placement
- Use lowest effective energy
- Continuous ECG and perfusion monitoring
- Re-interrogate device post-defibrillation
9. Intraoperative Indications for Defibrillator Pad Placement
- ICD present and therapies suspended
- History of VT/VF (secondary prevention)
- Pacing-dependent with expected EMI
- Leadless or subcutaneous ICD
- CRT device with no intrinsic rhythm
- Apply external pacing/defib pads and have defibrillator available
10. Special Considerations: Leadless PMs and Subcutaneous ICDs
Leadless Pacemakers (e.g., Medtronic Micra)
- Not easily reprogrammable
- Typically non-responsive to magnets
- Single-chamber pacing only
Subcutaneous ICDs
- No pacing capability
- Wide sensing vector → high EMI susceptibility
- Magnet suspends shock therapy only
Conclusion
- Always apply external pacing/defib pads preoperatively
- Monitor these patients in high-acuity settings
11. Identifying Pacemaker Dependence
- ECG: no underlying rhythm
- Device interrogation: no intrinsic activity
- Fixed HR (e.g., 60–65 bpm) without variability
- Clinical history: symptomatic bradycardia, AV node ablation
12. Preoperative Investigations
- ECG
- Chest X-ray
- Device interrogation report
- Echocardiogram (if CRT or known LV dysfunction)
- Blood tests: electrolytes, creatinine
- Confirm magnet response if needed
13. Magnet Use
Pacemaker
- Typically induces asynchronous pacing
ICD
- Suspends shocks only; pacing mode unaffected
Limitations
- Some devices do not respond to magnets
- Deep/obese tissue may reduce magnet efficacy
- Magnet use may be limited by sterile field
14. Intraoperative Monitoring
- Continuous ECG (preferably diagnostic mode)
- Pulse oximetry or invasive arterial monitoring
- Confirm mechanical systole
- Monitor for loss of capture or inhibition
15. Electrical Interference (EMI) – Sources and Management
Sources
- Monopolar diathermy
- Nerve stimulators
- Lithotripsy
- Central venous catheter (CVC) guidewire insertion
Management
- Use bipolar cautery where possible
- If monopolar needed:
- Use short bursts at lowest energy
- Ensure dispersive pad placed away from CIED
- Avoid underbody grounding
Links
References:
- Bryant, H. C., Roberts, P., & Diprose, P. (2016). Perioperative management of patients with cardiac implantable electronic devices. BJA Education, 16(11), 388-396. https://doi.org/10.1093/bjaed/mkw020
- Cardiothoracic Anaesthetic Society of South Africa. (2021). Perioperative management of patients with cardiac implantable electronic devices: 2021 statements and algorithms. Southern African Journal of Anaesthesia and Analgesia, 27(6 Suppl 1), S57–S63. https://doi.org/10.36303/SAJAA.2021.27.6.S1.2710
- Thomas, H., Plummer, C., Wright, I. J., Foley, P., & Turley, A. (2022). Guidelines for the peri‐operative management of people with cardiac implantable electronic devices. Anaesthesia, 77(7), 808-817. https://doi.org/10.1111/anae.15728
- Crossley GH. The Heart Rhythm Society (HRS)/American Society of Anesthesiologists (ASA) Expert Consensus Statement on the perioperative management of patients with implantable defibrillators, pacemakers and arrhythmia monitors. Heart Rhythm. 2011;8(7):1114-54. https://doi.org/10.1016/j.hrthm.2010.12.023
- The Calgary Guide to Understanding Disease. (2024). Retrieved June 5, 2024, from https://calgaryguide.ucalgary.ca/
- FRCA Mind Maps. (2024). Retrieved June 5, 2024, from https://www.frcamindmaps.org/
- Anesthesia Considerations. (2024). Retrieved June 5, 2024, from https://www.anesthesiaconsiderations.com/
- ICU One Pager. (2024). Retrieved June 5, 2024, from https://onepagericu.com/
Summaries:
ICU_one_pager_external_pacemakers_v11.pdf (squarespace.com)
ICD
Pacemakers
Copyright
© 2025 Francois Uys. All Rights Reserved.
id: “6009aedf-9800-413c-9b72-dd6b18ae23cc”



