- Overview (Groote Schuur Hospital Guidelines by Dr Dee Batty)
- Anaesthesia Guidelines for Hepatobiliary Surgery
- Thoracic Epidural Alternative (TEA Alternative)
- Postoperative High Care Management
{}
Overview (Groote Schuur Hospital Guidelines by Dr Dee Batty)
Anaesthesia Guidelines for Hepatobiliary Surgery
Thoracic Epidural Analgesia (TEA)
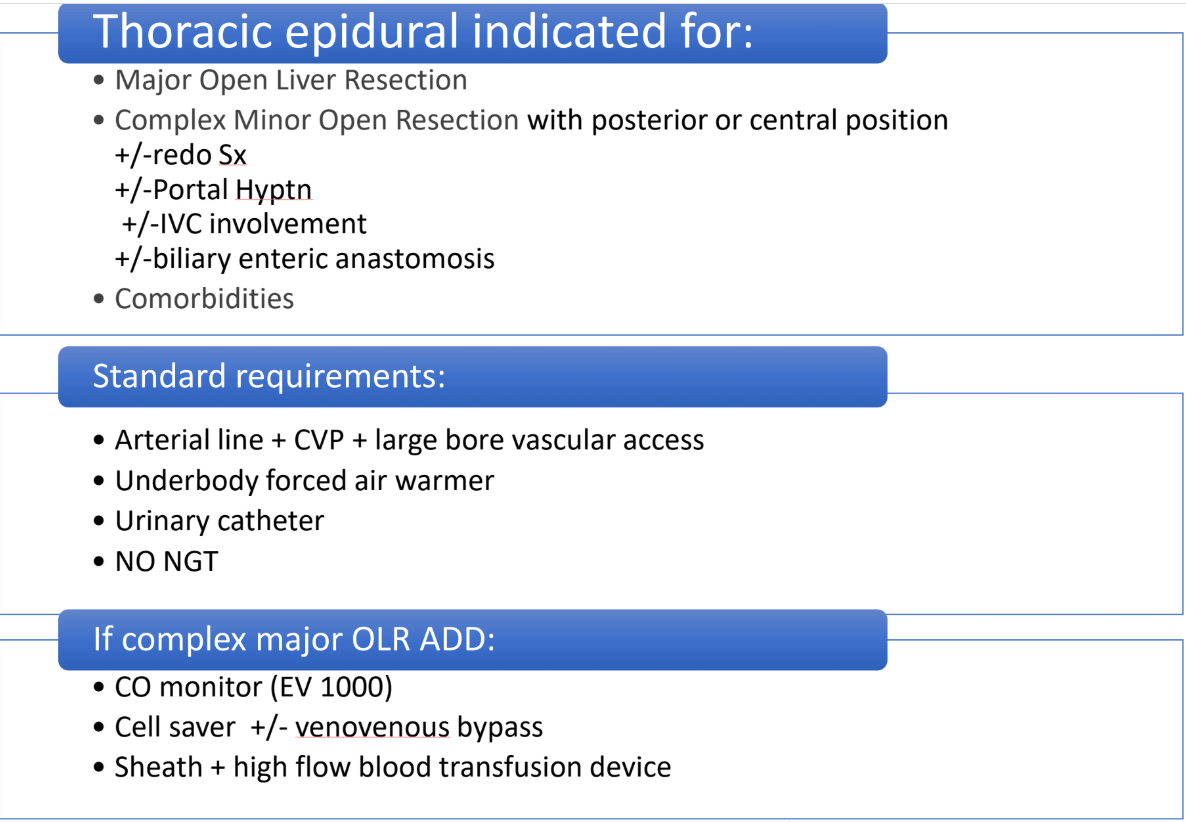
Indications
Major Open Liver Resection
- Complex minor resections involving:
- Posterior or central liver positions.
- Redo surgery.
- Portal hypertension.
- Inferior vena cava (IVC) involvement.
- Biliary-enteric anastomosis.
Comorbidities:
- Chronic obstructive airway disease (COAD) or other conditions where TEA assists in intraoperative and/or postoperative management.
Preoperative Preparation
-
Baseline Monitoring and Access
- Arterial line (A-line).
- Central venous pressure (CVP) monitoring.
- Large-bore vascular access.
-
Essential Equipment
- Underbody warming device.
- Urinary catheter.
-
Medications
- Prophylactic antibiotics (repeated every 4 hours).
-
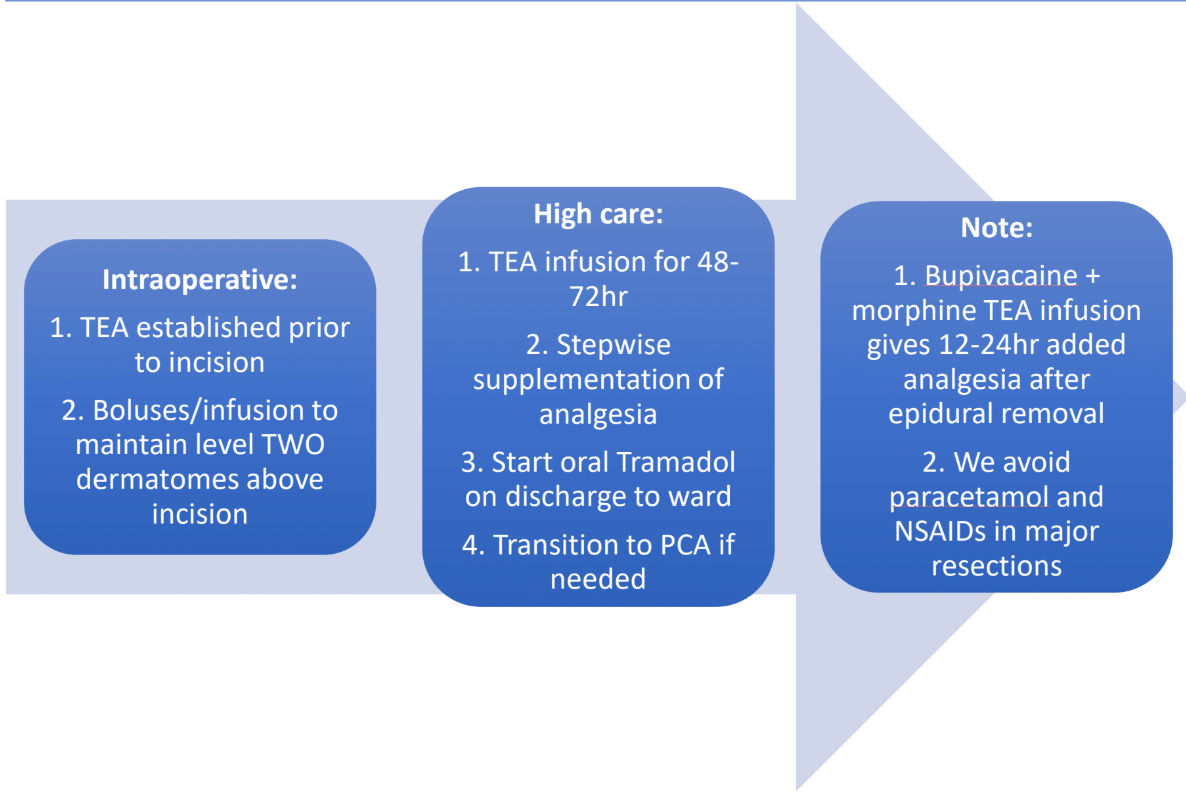
TEA Establishment
- Working epidural established pre-incision using bupivacaine 0.25%.
- Intraoperative boluses or continuous infusion to maintain a sensory block two dermatomes above the incision site.
Intraoperative Management
-
Fluid Management
- Employ fluid restriction combined with epidural-induced splanchnic and peripheral vasodilation to lower CVP until liver resection is complete.
-
Complex Major Open Liver Resection (OLR): Additional Measures
- Peripheral cardiac output monitoring (e.g., EV1000).
- Cell saver (± filter for cancer cases).
- Venovenous bypass (if indicated).
- Sheath placement and use of a high-flow blood transfusion and warming device (e.g., Ranger).
Postoperative Management
-
Analgesia
- Epidural infusion: Bupivacaine 0.1% with opioid infusion for 48–72 hours as per protocol.
- Supplement analgesia only as needed in a stepwise approach:
- Oral analgesia: Tramadol or Tapentadol on postoperative day (POD) 2 or 3 when transitioning to the ward.
- Consider patient-controlled analgesia (PCA) with fentanyl or morphine if additional control is required.
-
Adjuvant Medications
- Paracetamol and NSAIDs (if applicable), although typically avoided in major resections or complex minor resections.
Notes
- The bupivacaine/morphine infusion allows morphine accumulation, providing an additional 12–24 hours of analgesia post-TEA removal.
- Avoid paracetamol and NSAIDs in cases of major resections or complex minor resections to mitigate potential complications.
Thoracic Epidural Alternative (TEA Alternative)
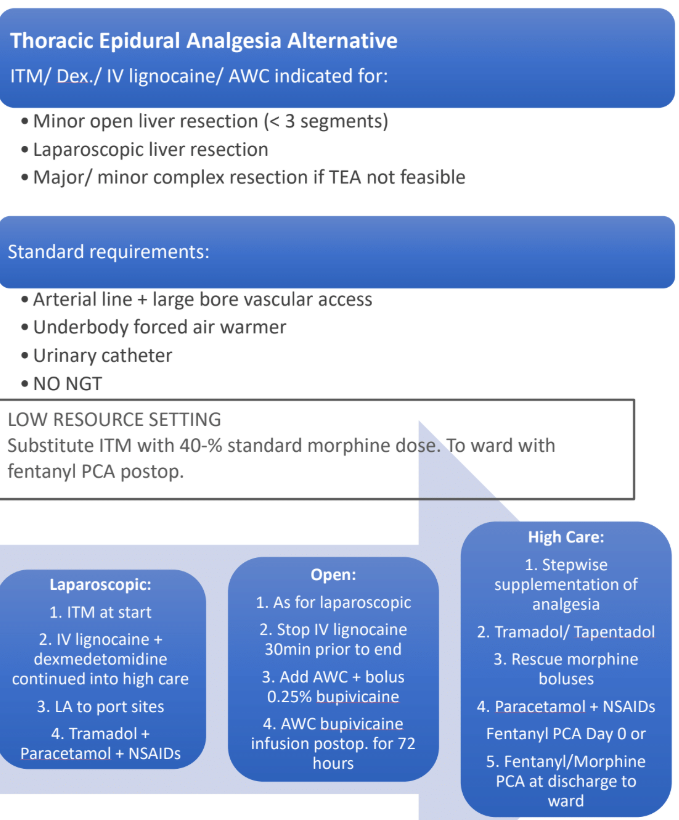
Indications for TEA Alternative
- Minor liver resections (involving fewer than three segments).
- Minor open liver resections.
- Laparoscopic liver resections.
- Major or complex minor resections if TEA is not possible or feasible.
Preoperative Preparation
-
Baseline Monitoring and Access
- Arterial line (A-line).
- Good vascular access (CVP monitoring not required).
-
Essential Equipment
- Underbody warming device.
-
Medications
- Prophylactic antibiotics, repeated every 4 hours.
-
Hemodynamic Management
- Fluid restriction combined with adjuvants to lower CVP appropriately until liver resection is completed.
Intraoperative Analgesic Approach
Laparoscopic Liver Resection
- Intrathecal Morphine (ITM): Administered at the start of the procedure.
- Intravenous Adjuvants:
- IV lignocaine and IV dexmedetomidine, initiated prior to incision and continued into postoperative high care for up to 24 hours.
- Local Analgesia:
- Local bupivacaine at port sites (*consider lignocaine dose in total dose calculation).
Conversion To Open Surgery
- IV Lignocaine: Discontinue 30 minutes before the end of the procedure.
- Wound Infusion Catheters (AWC): Placed at the end of surgery, administer:
- 0.25% bupivacaine bolus at placement (*consider lignocaine dose in total dose calculation).
- Continue bupivacaine infusion via AWC for up to 72 hours postoperatively.
Postoperative High Care Management
-
Oral Analgesics:
- Initiate as needed in a stepwise manner.
- Tramadol.
- Paracetamol and NSAIDs as appropriate (avoid in major or complex minor resections).
- Initiate as needed in a stepwise manner.
-
Systemic Opioid Use:
- Minimise systemic opiate use.
- Reserve morphine boluses for rescue analgesia only.
-
Patient-Controlled Analgesia (PCA):
- Day 0: Consider fentanyl PCA.
- Day 1 (24 hours post-spinal morphine): Transition to fentanyl or morphine PCA (+/- ketamine if needed).
-
Additional Considerations:
- Monitor for respiratory depression for 24 hours if ITM was used.
- In resource-limited settings lacking high-care beds, omit ITM and use IV morphine at approximately 40% of expected dose (adjuvants reduce total opioid requirements).
- If AWCs are unavailable:
- Use epidural catheters as wound infusion catheters.
- Insert one catheter into the posterior rectus sheath and one into the transversus abdominis plane (TAP). Attach to an electronic infusion pump for delivery.
Notes
- Avoid paracetamol and NSAIDs in major and complex minor resections. In minor resections, avoid NSAIDs if contraindicated.
- Consider all local anesthetic dosing (e.g., lignocaine and bupivacaine) when calculating maximum allowable dose to avoid toxicity.
Thoracic Epidural Analgesia (TEA)
Goals of TEA
- Preemptively establish a functioning epidural before incision.
- Maintain sensory block two dermatomes above incision level intraoperatively and postoperatively.
- Support splanchnic perfusion during the critical early period of liver regeneration (2–3 days postoperative).
Intraoperative Management
Fluid Management and Hemodynamic Goals
- Fluid restriction combined with epidural-induced splanchnic and peripheral vasodilation:
- Lowers CVP and facilitates portocaval decompression until liver resection is complete.
- Target Hemodynamics:
- MAP can safely decrease by up to 30% without compromising oxygen supply.
- Ideal parameters:
- MAP ~60 mmHg.
- HR ~60 bpm.
- Adjust targets based on patient-specific needs.
Pharmacologic Support for MAP
- Use IV phenylephrine for low MAP with high HR.
- Use IV ephedrine for low MAP with low HR.
Fluid Resuscitation Post-Hemostasis
- After achieving hemostasis:
- Return to normovolemia.
- Some centers initiate goal-directed fluid therapy (GDFT) with cardiac output monitoring at this point, continuing into the postoperative period.
Postoperative Management
Fluid Management
- Baseline Maintenance:
- Glucose-maintaining solution (GMS) at 1.2 ml/kg/hour.
- Rehydration:
- 1 L IV infusion over 24 hours.
- Boluses as Required:
- Use Voluven, Volulyte, or Balsol in 200 ml increments to maintain:
- Urine output: 0.3–0.5 ml/kg/hour.
- MAP > 60 mmHg.
- Use Voluven, Volulyte, or Balsol in 200 ml increments to maintain:
Fluid Therapy Notes
- GDFT (goal-directed fluid therapy):
- May optimize outcomes with stroke volume variation (SVV) and peripheral cardiac output monitoring.
- However, evidence from studies is inconclusive, and this may not be widely available.
- Avoid restrictive fluid policies to support liver regeneration, which requires increased cardiac output.
- Most patients can tolerate oral free fluids starting at 4 hours postoperative, progressing to full ward diet as tolerated.
Epidural Management
Postoperative Analgesia Protocol
- Always combine bupivacaine with an opiate (morphine or fentanyl unless contraindicated):
- Prevents tachyphylaxis and reduces escalating local anesthetic requirements.
Monitoring And Maintenance
- Sensory Level:
- Maintain level two dermatomes above incision using infusion and top-up boluses as needed.
- Adjust infusion rate early based on hourly checks for the first 3–4 hours, then every 4 hours.
- Motor Function:
- Monitor hourly for return of motor power initially, then every 4 hours once motor power has returned.
Safety Considerations
- Vigilantly monitor for epidural hematoma per established protocol.
TEA (Thoracic Epidural Analgesia) – How to Make It Work
Source: GSH and UCTPAH (2021)
Aims
- Provide an effective anaesthetic for a well-informed and cooperative patient.
- Establish the epidural block prior to incision and maintain a level two dermatomes above the incision (e.g., T4 for upper abdominal surgery).
- Transition seamlessly into the postoperative phase with a continuous infusion of 0.1% bupivacaine plus an opioid for:
- Maximal pain relief.
- Neural deafferentation.
- Minimal side effects.
- Avoid intravenous opioids except during the transition from epidural to IV morphine infusion or PCA.
- Educate patients about risks without causing undue anxiety, emphasizing protocols to detect and manage complications.
Technique
Patient Positioning
- Positioning contributes 90% to the success of the epidural.
- Use anxiolysis with midazolam titrated to achieve a cooperative patient.
Epidural Level
- Ideal level: T9–T10 for upper abdominal surgery (advantage of horizontal needle insertion).
- Avoid higher levels (e.g., T7–T8) unless required; higher insertion does not significantly improve the block and may cause urinary catheter discomfort.
Sterile Preparation
- Use chlorhexidine with alcohol and allow it to dry.
- Full sterile precautions: Mask, gloves, cap, gown.
Epidural Catheter Placement
- Use loss of resistance (LOR) with saline.
- Insert multi-orifice catheter 5–7 cm into the epidural space (do not advance further to minimize vessel infiltration risk).
- Test dose: 2 ml of 2% lignocaine to confirm proper placement.
Intraoperative Management
Block Establishment
-
Preemptive Blockade:
- Use a bupivacaine-lignocaine mix (e.g., 7 ml of 0.5% bupivacaine + 3 ml of lignocaine).
- Sensory level (T4) achieved within 3–4 minutes.
- Volume required: 12–20 ml total for a T4 block (to cover ~2–6 dermatomes above the incision level).
-
“Paint the Fence” Technique:
- Administer half the total calculated volume 30 minutes before incision to increase block density.
- _Skip this step if cardiovascular instability exists or time is constrained; instead, give the first hourly volume 1 hour post-insertion.
-
Maintenance:
- Administer 4/5 of the original volume hourly:
- Bolus or infusion with 0.25% bupivacaine intraoperatively.
- Start infusion immediately after the first bolus (at 1 hour).
- Do not stop boluses or infusion intraoperatively. Support blood pressure with:
- IV fluid boluses.
- Ephedrine or low-dose phenylephrine if required.
- Administer 4/5 of the original volume hourly:
-
Local Anaesthetic Around Drains:
- Apply local anaesthetic to drain sites before the procedure concludes.
Postoperative Management
Infusion
- Continue the intraoperative infusion rate using 0.1% bupivacaine plus an opioid of choice (e.g., morphine or fentanyl).
Monitoring
- First 2–3 hours: Check sensory level hourly to ensure a steady state. Adjust the infusion rate early if required.
- Top-ups:
- Use 0.25%–0.5% bupivacaine to increase block density or raise the sensory level.
- Bolus 3–5 ml every 5 minutes as needed, up to the total original dose.
- Wait too long between boluses, and block density increases without raising the sensory level.
Blood Pressure Support
- Blood pressure instability is uncommon (if the patient is not fluid-deficient) after 3–4 hours of a well-established block.
- Use IV fluid boluses or ephedrine if required to support blood pressure.
Local Anaesthetic Use
- Mechanism: Blocks afferent and efferent signals, suppressing the surgical stress response. Facilitates:
- Return of gastric motility.
- Reduction in inflammation.
- Decreased blood viscosity.
- Dosing:
- Postoperative infusion rates up to 25 ml/hour of 0.1% bupivacaine are acceptable, provided total bupivacaine dose does not exceed 2 mg/kg/4 hours.
- Agent Selection:
- Bupivacaine, levobupivacaine, ropivacaine are all effective.
- Clinical advantages (e.g., less cardiotoxicity, reduced motor block) of levobupivacaine and ropivacaine are minimal at the low doses used.
Opioids In TEA
- Mechanism: Act synergistically with local anaesthetics, reducing the required concentration of LA.
- Selection and Effects:
- Morphine (hydrophilic):
- Slower onset (30–60 minutes).
- Extensive CSF spread, leading to delayed respiratory depression.
- Long duration (6–24 hours).
- Fentanyl/Sufentanil (lipophilic):
- Rapid onset (5–10 minutes).
- Limited CSF spread and shorter duration (2–4 hours).
- Most of the drug exerts systemic effects rather than spinal action due to low bioavailability at the dorsal horn.
- Morphine (hydrophilic):
Postoperative Infusion Example
- Morphine Infusion:
- Concentration: 0.05 mg/ml morphine + 0.1% bupivacaine (10 mg morphine + 200 ml 0.1% bupivacaine).
- Dose: 6–15 ml/hour (300–750 µg/hour morphine).
- Start intraoperatively or immediately postoperatively.
Advantages of Morphine Infusion
- Accumulated CSF morphine provides up to 24 hours of analgesia after stopping the infusion, easing transition to oral analgesics.
- Reduced total dose minimizes side effects (e.g., respiratory depression, nausea, pruritus).
TEA Alternative Strategy
Aim
To replicate the following benefits of thoracic epidural analgesia (TEA):
- Analgesia: Via ITM (intrathecal morphine), dexmedetomidine (DEX), and lignocaine.
- CVP Lowering: Through DEX and fluid restriction.
- Stress Reduction: By minimizing hemodynamic disturbances.
- Immunomodulation: Utilizing DEX and lignocaine.
Technique
Monitoring and Access
- Nasogastric Tube (NGT): Not required.
- Arterial Line (A-line): Routine for continuous hemodynamic monitoring.
- Central Venous Pressure (CVP):
- Required for:
- Hepatectomy, extended hepatectomy, or complex segmentectomy.
- Central liver resections, proximity to major vessels, redo surgeries.
- Cases with portal hypertension, biliary-enteric anastomosis, or sepsis risk.
- Not required for:
- Laparoscopic resections.
- Simple minor liver resections.
- Alternatives: Use stroke volume variation (SVV) as a surrogate for CVP. Requires a peripheral cardiac output monitor attached to the A-line. Useful for goal-directed fluid therapy (GDFT) in major or complex open liver resections (OLR) if available.
- Required for:
Fluid Management
- Restrict fluids to maintain low CVP until liver resection and hemostasis are complete.
Anaesthesia Plan
IV Access
- Large Bore IV Access: 14G–16G.
- Second Peripheral Line: For drug infusions (DEX, lignocaine, phenylephrine).
Intrathecal Morphine (ITM)
- Dose: 150–250 µg, diluted to 1.5–2 ml with saline.
- Optional Addition:
- Plain bupivacaine (3–4 ml): If stable hemodynamics and surgery duration >3–4 hours are expected.
- Adequate volume required to provide coverage for the upper abdominal incision.
- Slow onset contributes to hemodynamic stability.
- Note: ITM provides 12–24 hours of postoperative analgesia but is not sufficient for intraoperative surgical analgesia.
Dexmedetomidine (DEX)
- Concentration: 4 µg/ml.
- Infusion Rate: 0.1–0.5 µg/kg/hour, titrated to effect (target HR ~60 bpm, MAP ~60 mmHg).
- Optional Bolus: Up to 0.5 µg/kg at initiation.
- Avoid:
- Large boluses (e.g., 1 µg/kg) due to risk of hypertension and bradycardia via α2B receptor activation.
IV Lignocaine
- Loading Dose: 1.5 mg/kg over 10 minutes.
- Infusion Rate: 1 mg/kg/hour.
- Duration: Continue until 30 minutes prior to the end of surgery.
Intraoperative Opioids
- Fentanyl: 200–400 µg during the procedure.
- Morphine: Optional early administration (approximately 40% of the usual anticipated dose).
- Note: IV DEX and lignocaine reduce intraoperative opioid requirements by up to 50%.
Postoperative Analgesia
Analgesic Benefits
- ITM provides significant postoperative pain relief for 12–24 hours.
- Respiratory depression risk with ITM: 0.3–3%.
Respiratory Considerations
- Increased risk of respiratory depression when combining:
- Spinal morphine.
- Parenteral opioids.
- Sedatives (e.g., dexmedetomidine).
Wound Infusion Catheters
- Single catheter:
- Use 0.2% bupivacaine.
- Double catheter for midline incisions:
- Administer 0.2% bupivacaine at 5 ml/hour per catheter (or 8 ml/hour total via a splitter).
Dexmedetomidine
- Continue infusion in high care: 0.1–0.3 µg/kg/hour.
Stepwise Supplementation
- Oral analgesics:
- Tramadol or Tapentadol.
- As appropriate:
- Paracetamol (IV or oral).
- NSAIDs (IV or oral), only if indicated and appropriate for patient condition.
- For breakthrough pain:
- Morphine boluses as needed.
- Fentanyl PCA can be used but is usually deferred until Day 1 during transition to the ward.
Respiratory Monitoring
Monitoring Schedule
- First 12 hours: Hourly assessment of respiratory rate and level of consciousness.
- Next 12 hours: Every two hours.
- Additional Monitoring:
- Continuous pulse oximetry.
- ABG analysis for CO₂ monitoring, if indicated.
Risk Factors for Respiratory Depression
Pharmacological Factors
- Higher intrathecal morphine doses.
- Systemic opiate co-administration.
- Co-administration of sedatives or magnesium.
Patient-Specific Factors
- Advanced age, female sex.
- Conditions: OSA, COPD, obesity, diabetes mellitus, cardiac/neurological/renal disease, opioid dependence.
Treatment for Respiratory Depression
- Administer low-dose naloxone infusion for up to 12 hours if required.
Fluid Management
Maintenance Fluids
- GMS IVI: 1.2 ml/kg/hour.
- Rehydration: 1 liter IVI over 24 hours.
Volume Boluses (as needed)
- Use Voluven, Volulyte, or Balsol in 200 ml increments to maintain:
- Urine output: 0.3–0.5 ml/kg/hour.
- MAP > 60 mmHg.
Fluid Strategy Based on Resection Type
- Major Resections: Follow the TEA guideline approach (avoid restrictive fluid policies).
- Minor Resections: Maintain normovolemia with minimal reliance on volume boluses
Use Of NSAIDs and Paracetamol
Recommendations
- Both are supported by ERAS and Prospect guidelines for liver resection analgesia.
- Their use depends on:
- Extent of liver resection.
- Liver condition (e.g., cirrhosis, fatty liver, recent chemotherapy, ischemic insult).
- Comorbidities.
Contraindications for NSAIDs
- Absolute:
- Elderly patients, peptic ulcer disease, gastritis.
- Hypertension, cardiovascular disease, renal insufficiency.
- Cox-2 Inhibitors:
- Contraindicated in ischemic heart disease (IHD), stroke, and renal impairment.
- Relative (Use with caution):
- Hypertension, hyperlipidemia, diabetes, peripheral artery disease.
- Smokers, patients at risk for AKI, or those with stress ulceration.
Administration
- Use the lowest effective dose for the shortest duration (<5 days perioperatively).
Links
Pancreatoduodenectomy (Whipple’s procedure)
References
- Batty, D. (2021). Guidelines for Anaesthesia for Hepatobiliary Surgery: GSH and UCTPAH. Unpublished institutional guidelines, Groote Schuur Hospital and University of Cape Town Private Academic Hospital.
id: “2085cef2-52fd-4728-8bf5-b9c8774f7d33”



