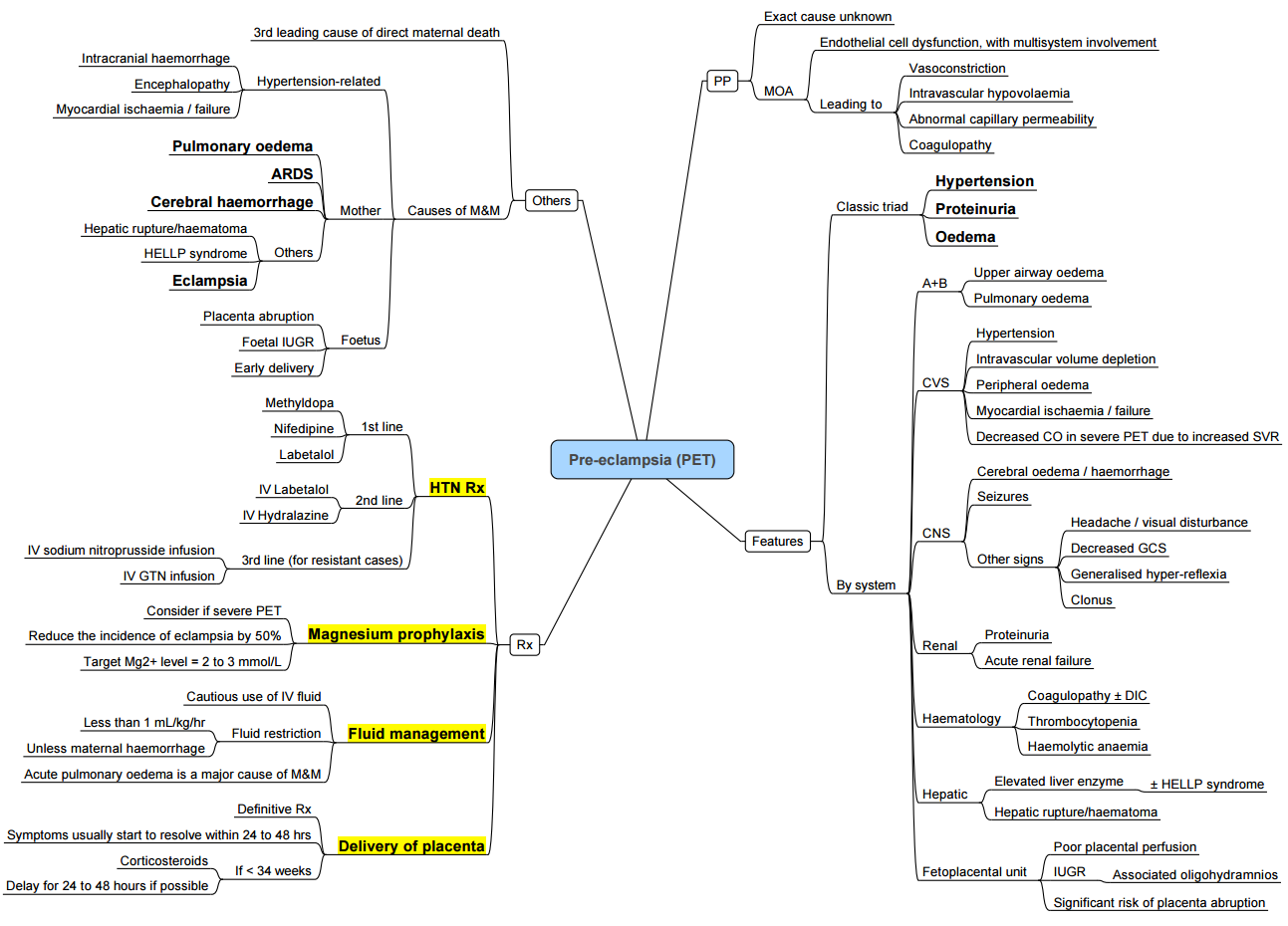
- Summary of PET
- Treatment Options
- Perioperative Management
- Links
- Past Exam Questions
{}
Summary of PET
Introduction
- Preeclampsia is a multisystem disorder unique to human pregnancy, characterised by new‑onset hypertension and organ dysfunction after 20 weeks of gestation. Hypertensive disorders affect approximately 5–10% of all pregnancies worldwide, contributing significantly to maternal and perinatal morbidity and mortality.
Incidence and Impact
- Global prevalence: Hypertensive disorders complicate 5–10% of pregnancies; preeclampsia accounts for 2–8%.
- Maternal mortality: Responsible for ~14% of maternal deaths globally and up to 20% in low‑resource settings.
- Long‑term risks: Women with a history of preeclampsia have a twofold increase in future hypertension and cardiovascular disease, and a threefold increase in end‑stage renal disease.
- Neonatal outcomes: Associated with fetal growth restriction, preterm delivery, perinatal mortality and increased lifetime cardiovascular risk in offspring.
Classification of Hypertensive Disorders
- Chronic hypertension: Present before pregnancy or diagnosed before 20 weeks; may be complicated by superimposed preeclampsia (new endorgan dysfunction as below.)
- Or persistent hypertension for >12 weeks post partum
- Gestational hypertension: New‑onset hypertension (systolic ≥ 140 mmHg or diastolic ≥ 90 mmHg) after 20 weeks without proteinuria or end‑organ dysfunction; 15–25% progress to preeclampsia.
- Not recommended to start treatment for hypertension unless >160/110 mmHg.
- Does not prevent progression to preeclampsia
- Not recommended to start treatment for hypertension unless >160/110 mmHg.
- Preeclampsia: Gestational hypertension with one or more of:
- Proteinuria (≥ 300 mg/24 h or protein/creatinine ratio ≥ 0.3).
- Other organ dysfunction (e.g. renal insufficiency, liver enzyme elevation, neurological features, haematological disturbances).
- Severe features: Any of:
- Severe hypertension (systolic ≥ 160 mmHg or diastolic ≥ 110 mmHg).
- Thrombocytopenia (platelets < 100 × 10⁹/L).
- Impaired liver function (transaminases > × 2 normal).
- Progressive renal insufficiency (creatinine > 90 µmol/L).
- Pulmonary oedema or new neurological signs.
Anaesthetic Implications
- Blood pressure control: Aim for systolic 140–150 mmHg and diastolic 90–100 mmHg; first‑line agents include labetalol and hydralazine, with nitroprusside reserved for emergencies.
- Monitoring: Invasive arterial line for continuous blood pressure monitoring in severe disease; central venous access if significant haemodynamic instability suspected.
- Neuraxial anaesthesia: Platelet count ≥ 75 × 10⁹/L generally acceptable; avoid if < 70 × 10⁹/L or with coagulopathy.
- Airway management: Anticipate difficult airway due to oropharyngeal oedema; prepare for smaller endotracheal tube and difficult extubation.
- Seizure prophylaxis: Magnesium sulphate regime: loading dose 4 g IV over 20 min followed by infusion 1 g h⁻¹ for at least 24 h postpartum.
- Fluid management: Avoid excessive crystalloids; judicious use guided by invasive monitoring to reduce risk of pulmonary oedema.
Pathophysiology
- A two‑stage model:
- Abnormal placentation: Inadequate cytotrophoblast invasion leads to high‑resistance uteroplacental circulation.
- Maternal syndrome: Release of antiangiogenic factors (sFlt‑1, soluble endoglin) induces widespread endothelial dysfunction, vasoconstriction and capillary leak.
Systemic Manifestations
| System | Manifestations |
|---|---|
| Neurological | Headache, visual disturbance, hyperreflexia, eclampsia |
| Respiratory | Pulmonary oedema, reduced functional residual capacity |
| Cardiovascular | Severe vasospasm, left ventricular dysfunction |
| Renal | Proteinuria, oliguria, rising creatinine |
| Hepatic | RUQ pain, transaminase elevation, HELLP syndrome |
| Haematological | Thrombocytopenia, haemolysis, DIC |
| Feto‑placental | Growth restriction, abnormal Dopplers, risk of abruption |
Complications
Acute
- Maternal: abruptio placentae; pulmonary oedema; acute kidney injury; liver failure; intracerebral haemorrhage or infarction secondary to loss of autoregulation and increased capillary permeability; progression to eclampsia with cytotoxic and/or vasogenic cerebral oedema (commonest cause of mortality).
- Neonatal: preterm birth; fetal growth restriction; hypoxic‑ischaemic encephalopathy; perinatal death.
- Risk factors for eclampsia: primiparity; young maternal age (<20 years) or >35y; low body mass index; high diastolic at booking, previous PET
Chronic
- Persistent left ventricular diastolic and/or systolic dysfunction may continue for ≥1 year after early‑onset disease.
- ↑ long‑term risk of chronic hypertension (11–14% within 10 years), ischaemic heart disease, cerebrovascular events, venous thromboembolism, white matter lesions and end‑stage renal disease.
- Cognitive deficits (impaired memory and verbal learning) may persist >15 years.
HELLP Syndrome
- Hemolysis evidence (any of):
- Serum LDH > 600 U L⁻¹ or total bilirubin > 1.2 mg dL⁻¹
- Peripheral-blood smear showing schistocytes or burr cells
- Low haptoglobin (<25 mg dL⁻¹) or rising reticulocyte count
- Elevated liver enzymes: aspartateor alanine-aminotransferase (AST/ALT) ≥ 70 IU L⁻¹ or ≥ 2 × upper-limit-of-normal
- Low platelet count: < 100 × 10⁹ L⁻¹
- Diagnostic rule: Complete HELLP = all three triad components present; partial HELLP = severe pre-eclampsia plus one or two components (e.g., ELLP, EL)
Cardiac Complications in Preeclampsia
Overview
- Spectrum: heart failure (HFpEF > HFrEF), pulmonary oedema, myocardial ischaemia, myocardial oedema, pericardial effusion.
- HFpEF: commonest (up to 10% in severe disease); often iatrogenic (excess fluid load); key contributor to ICU admissions and mortality.
- HFrEF: less frequent; presents with hypotension, tachycardia; high risk of decompensation.
Assessment
- Echocardiography: transthoracic echo for systolic/diastolic function, ventricular dimensions, pericardial fluid; use rapid obstetric screening echo (ROSE) for bedside evaluation.
- Biomarkers: NT‑proBNP (upper limit 200 pg/mL in 1st–2nd trimester, 150 pg/mL in 3rd); BNP (<50 pg/mL).
- Differential: distinguish from peripartum cardiomyopathy (EF < 45% without hypertension) to guide prognosis and counselling.
Echo Findings in Preeclampsia
- Global left-ventricular systolic function: visually estimated or Simpson biplane EF; normal adult range ≈ 53–73 %
- Diastolic dysfunction patterns: elevated E/e′ > 14, E/A < 0.8 (grade I) or > 2 (grade III), DT < 160 ms, TR ≥ 2.8 m s⁻¹
- Regional wall-motion abnormality (RWMA): hypo/akinesia or dyskinesia in a coronary territory → acute ischaemia or infarction
- Left-ventricular hypertrophy: septal or posterior wall thickness > 12 mm (concentric) or end-diastolic diameter > 58 mm (eccentric)
- Left-atrial enlargement: volume index > 34 mL m⁻² or antero-posterior diameter > 4.0 cm suggests chronic pressure/volume load
- Right-ventricular dilatation & “D-shaped” LV: basal RV diameter > 42 mm plus septal flattening → pulmonary hypertension or RV pressure overload
- TR jet velocity ≥ 3.4 m s⁻¹: echoes a systolic pulmonary-artery pressure > 50 mm Hg
- Pericardial effusion/tamponade: anechoic space > 15 mm plus right-atrial systolic or right-ventricular diastolic collapse and plethoric IVC
Management
HFpEF
- BP reduction: IV glyceryl trinitrate 5 µg/min, titrate q3–5 min to max 100 µg/min.
- Diuresis: IV furosemide 20–40 mg IV bolus over 2 min; repeat to total 120 mg/h as needed.
- Symptom relief: morphine 2–5 mg IV.
- Respiratory support: CPAP/BiPAP or high‑flow nasal oxygen; invasive ventilation if indicated.
- Fluid restriction: limit to maintenance rates to prevent overload.
HFrEF
- Inotropes: dobutamine or milrinone as per haemodynamic indices.
- Cardiac arrest: follow Also algorithm; consider perimortem Caesarean section ≤5 min post‑arrest.
Multidisciplinary Care
- Collaborative team: obstetrician, anaesthetist, cardiologist, intensivist, neonatologist.
- Early echo, ICU transfer, and joint planning optimise outcomes.
Treatment Options
| Drug / Route (typical indication) | Guideline dose & escalation | Maximum dose | Common maternal side-effects | Key contraindications / cautions |
|---|---|---|---|---|
| Labetalol IV (acute severe HTN) | 10–20 mg bolus → 20–80 mg every 10–30 min; or 1–2 mg min⁻¹ infusion | 300 mg cumulative | Bradycardia, nausea, scalp tingling | Asthma, ≥1° heart block, decompensated HF, severe bradycardia |
| Labetalol oral (maintenance) | Start 200 mg 12-hourly; double every 12 h as needed | 2 400 mg day⁻¹ | Fatigue, fetal/neonatal bradycardia, hepatotoxicity (rare) | Same as IV; monitor LFTs in prolonged use |
| Nifedipine IR oral (acute severe HTN) | 10–20 mg; repeat in 20 min; then 10–20 mg every 2–6 h | 180 mg day⁻¹ | Headache, flushing, reflex tachycardia | Severe aortic stenosis; cautious co-administration with MgSO₄ (hypotension) |
| Nifedipine MR oral (chronic/post-partum) | 30–60 mg daily (XR); titrate q7 days | 120 mg day⁻¹ | Peripheral oedema, dizziness | Same as above |
| Hydralazine IV (acute severe HTN) | 5–10 mg bolus (IV/IM); repeat every 20–40 min; infusion 0.5–10 mg h⁻¹ | 20 mg cumulative | Maternal hypotension, tachycardia, headache, drug-induced lupus | Tachycardia-induced myocardial ischaemia, systemic lupus erythematosus flare |
| Methyldopa oral (chronic) | 250 mg 8–12-hourly for 48 h; titrate by 250 mg every 2 days | 3 g day⁻¹ | Sedation, dry mouth, positive Coombs test, hepatotoxicity | Active hepatitis, autoimmune haemolytic anaemia, depression |
| Nicardipine IV infusion (refractory severe HTN) | 2–6 mg h⁻¹, weight-based titration | 15 mg h⁻¹ (institutional) | Headache, flushing, hypotension, pulmonary oedema | Significant LV failure; caution in pulmonary oedema risk |
| Nitroglycerin IV infusion (HTN + pulmonary oedema) | Start 5–10 µg min⁻¹; ↑ by 5 µg min⁻¹ q3–5 min | 200 µg min⁻¹ (short term) | Severe headache, hypotension, reflex tachycardia | RV infarction, hypertrophic cardiomyopathy, PDE-5 inhibitor use within 24 h |
| Sodium nitroprusside IV (last-resort) | 0.5–4 µg kg⁻¹ min⁻¹; titrate to effect | 10 µg kg⁻¹ min⁻¹ (≤10 min) | Cyanide/thiocyanate toxicity, reflex tachycardia, hypotension | Pregnancy generally contraindicated—fetal cyanide toxicity; avoid in renal/hepatic impairment |
- First-line choices: Start with IV labetalol, IV hydralazine, or oral immediate-release nifedipine for acute BP ≥ 160/110 mm Hg; choose based on maternal comorbidities (e.g., avoid labetalol in asthma). For chronic or postpartum control, oral labetalol, modified-release nifedipine, or methyldopa are preferred.
- Escalation: If BP remains uncontrolled after two first-line boluses/infusion titrations, proceed to continuous nicardipine.
- Special situations: Add nitroglycerin when pulmonary oedema complicates pre-eclampsia; reserve nitroprusside for life-threatening, refractory crises under ICU and foetal monitoring with concurrent sodium thiosulphate
Perioperative Management
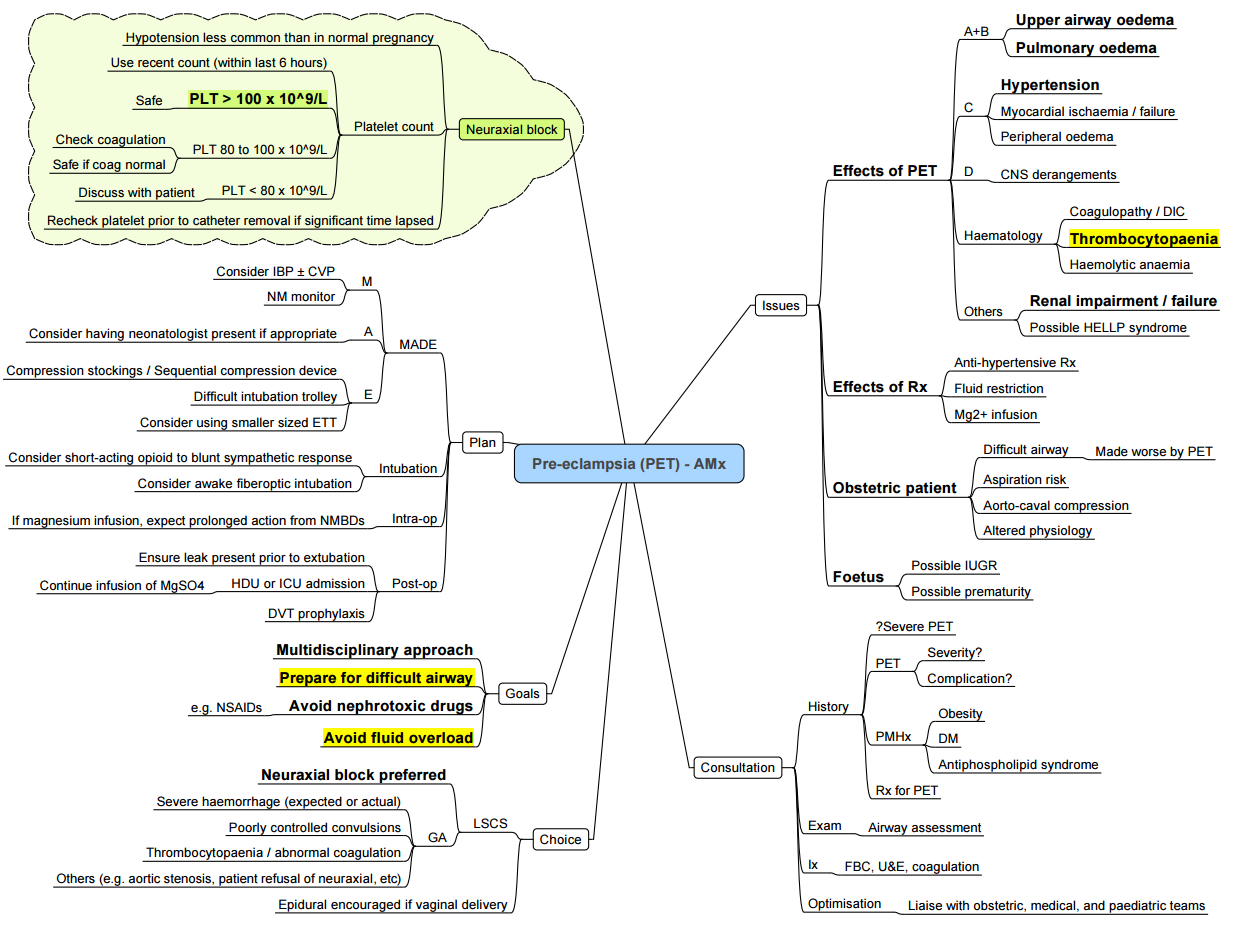
Perioperative Management
Preoperative
- Aspirin prophylaxis: 75–150 mg daily from 12–16 weeks until 36 weeks; not a contraindication to neuraxial anaesthesia.
- Calcium: 1 000 mg daily if dietary intake <1 000 mg/day; not routine in high‑income settings.
- Glucocorticoids: betamethasone or dexamethasone for fetal lung maturation if <34 weeks.
- Multidisciplinary planning: determine optimal timing, location and team composition for delivery.
- Blood testing interval
- 6 hourly: Preeclampsia
- 2 hourly: Preeclampsia with severe features/ HELLP
- Optimize BP to less than 150/80-100 prior to anaesthetic (slow reduction)
Intraoperative
Monitoring
- Arterial line: beat‑to‑beat BP; blood sampling.
- Echo-guided volume: transthoracic or TOE for volume/resistance assessment.
- Avoid routine CVP/PA catheters: limited benefit in PET.
Anaesthesia Choice
- Neuraxial: spinal, epidural or CSE preferred; platelet ≥80 × 10⁹/L; treat hypotension with phenylephrine (25–50 µg) or ephedrine (2.5–5 mg).
- General: indicated for coagulopathy, thrombocytopenia <70 × 10⁹/L, haemodynamic instability, refusal; plan RSI with video‑laryngoscope, minimise hypertensive surges during laryngoscopy and extubation.
Fluid & Haemorrhage
- Fluid: restrict to 80 mL/h maintenance or 1ml/kg/hour; guided by pulse pressure variation, urine output or echo.
- Haemorrhage risk: ~25% in PET; correct anaemia; use oxytocin/carbetocin; viscoelastic testing for coagulopathy.
Seizure Management
- Load Mgs04 as per guideline
- Give 2g after each seizure
Conversion to GA
- Preparation: anticipate and mitigate airway oedema; ensure resuscitation (fluids, blood) complete; team support; clear communication.
Decision Algorithm for Spinal Vs General Anaesthesia (SA Guideline)
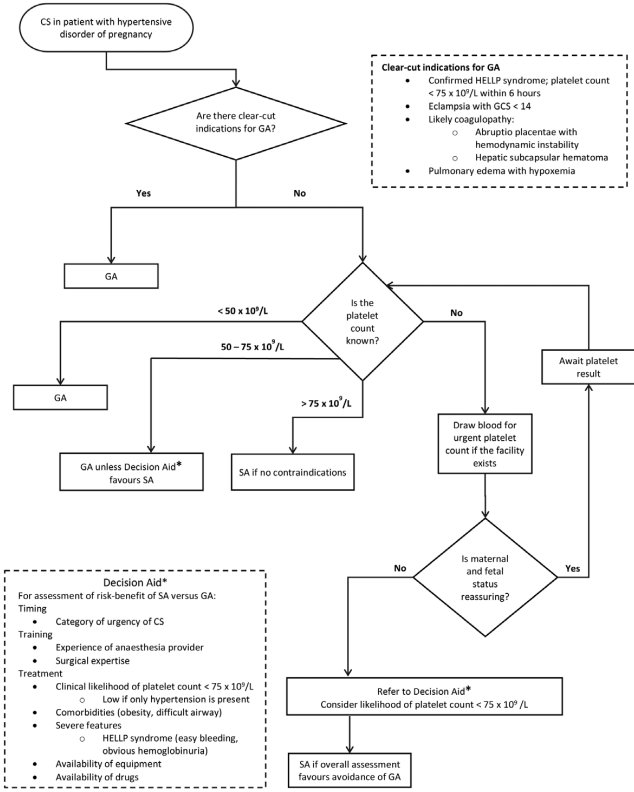
Recommendations for Anaesthesia in Eclampsia
Indications for Spinal Anaesthesia
- GCS ≥ 14; platelets >75 × 10⁹/L; no airway/ICP concerns.
Clear-Cut Indications for General Anaesthesia
- HELLP with platelets <75 × 10⁹/L; GCS <14; ≥2 seizures or focal signs; suspected coagulopathy (abruption, hepatic haematoma); pulmonary oedema with hypoxaemia.
Decision Pathway
- Any GA indication → GA
- No GA indication → check platelets:
- <50 × 10⁹/L → GA
- 50–75 × 10⁹/L → GA unless neuraxial benefit clearly outweighs risk
- More than 75 × 10⁹/L → spinal if no other contraindications
- Reassess maternal–fetal status; non‑reassuring → GA
Magnesium Protocol
- Magnesium sulfate (MgSO₄) is the first-line anticonvulsant for severe pre-eclampsia and eclampsia. A full course begins with a 4 g IV loading dose (or 10 g IM split 5 g per buttock) followed by a 1 g h⁻¹ continuous infusion—or 5 g IM every 4 h—for 24 h after the last seizure or delivery.
- Randomised data show the 1 g h⁻¹ rate is as effective as higher rates with fewer adverse effects.
- If a convulsion recurs, give an extra 2–4 g IV bolus over 5 min and continue the same maintenance. Monitor patellar reflexes, respiratory rate > 12 min⁻¹, and urine output > 25 mL h⁻¹; treat toxicity with 1 g (10 mL) IV calcium gluconate.
- Post-partum blood pressure often peaks on days 3–6, so keep antihypertensives, continue seizure prophylaxis for at least 24 h, and provide clear “red-flag” instructions before discharge.
Loading (initial) Regimen
| Route | Dose & rate | Practical preparation | Key points |
|---|---|---|---|
| IV (preferred) | 4 g (8 mL of 50 % MgSO₄) diluted to 20 mL; give over 5–15 min via pump or slow push | Draw 8 mL (4 g) from a 50 % ampoule (500 mg mL⁻¹) and add 12 mL 0.9 % NaCl | Rapid control, easy titration |
| IM (if no pump / poor IV access) | 10 g total: 5 g (10 mL of 50 %) deep IM each buttock with 1 mL 2 % lignocaine | Use a 21-G, 38-mm needle; massage site | Painful; ensure ambulation safety |
| Combined (Pritchard) | 4 g IV as above plus 10 g IM (5 g each side) | Gives rapid serum level and depot | Standard in many low-resource protocols |
When to Repeat a Loading Bolus
- Give 2–4 g IV over 5 min if the woman convulses again during maintenance, or if serum Mg²⁺ < 2 mmol L⁻¹ and clinical signs permit.
2. Maintenance Infusion
| Regimen | Preparation example | Administration | Evidence |
|---|---|---|---|
| 1 g h⁻¹ IV (Zuspan) | Add 20 g MgSO₄ (40 mL of 50 %) to 1 L RL = 20 mg mL⁻¹ (2 %) → 50 mL h⁻¹ delivers 1 g h⁻¹ | Infuse for 24 h after last fit/delivery; adjust to 0.5–2 g h⁻¹ if renal impairment or obesity | 1 g h⁻¹ non-inferior to 2 g h⁻¹, with fewer hot flushes and respiratory depression |
| 5 g IM q4 h (Pritchard) | 5 g (10 mL 50 %) + 1 mL lignocaine each buttock alternately | Start 4 h after loading; continue for 24 h | Use where pumps are unavailable |
- Stop the infusion only if: reflexes disappear, RR < 12 min⁻¹, urine output < 25 mL h⁻¹, or Mg²⁺ ≥ 3.5 mmol L⁻¹. Restart when parameters normalise.
3. Monitoring and Toxicity
| Parameter | Target / action | Rationale |
|---|---|---|
| Patellar (or biceps) reflex | Present | First sign of excess drug |
| Respiratory rate | ≥ 12 min⁻¹ | Respiratory-centre suppression precedes arrest |
| Urine output | ≥ 25–30 mL h⁻¹ | Renal clearance prevents accumulation |
| Serum Mg²⁺ (if available) | 2.0–3.5 mmol L⁻¹ (therapeutic range) | > 5 mmol L⁻¹ → risk of apnoea or cardiac block |
| Antidote | 10 mL 10 % Ca-gluconate IV over 3 min | Reverses respiratory or cardiac toxicity |
- Signs of toxicity include loss of reflexes (Mg²⁺ ≈ 3.5 mmol L⁻¹), respiratory depression (≈ 5 mmol L⁻¹), and cardiac arrest (≈ 6 mmol L⁻¹).
Management of a Post-eclampsia Fit (post-partum or antenatal)
- Call for help; place the woman in left lateral tilt and protect airway.
- Give oxygen 10–15 L min⁻¹ via NRB mask and secure IV access.
- Administer MgSO₄ loading (see Section 1). If on maintenance, give an extra 2 g IV
- Control severe hypertension (SBP ≥ 160 or DBP ≥ 110 mm Hg) with IV labetalol 10–20 mg or hydralazine 5–10 mg.
- Check glucose, electrolytes, FBC, creatinine, and consider CT/MRI if neuro-deficit persists (exclude intracranial bleed or PRES).
- Continue maintenance infusion for 24 h after the last fit (not the first).
Post-partum (“fourth-trimester”) Considerations
- Hypertension rebounds on days 3–6; arrange home BP monitoring and maintain antihypertensives for at least 7 days.
- Seizures can occur up to 6 weeks; advise urgent review for headache, visual aura, epigastric pain, or dyspnoea.
- Breast-feeding is safe; infant Mg²⁺ exposure is minimal.
Postoperative Management
Immediate Monitoring and Location of Care
- Care Setting: Transfer to high‑dependency or ICU for severe preeclampsia; enhanced obstetric unit for mild–moderate cases
- Vital Signs: BP, HR, RR, SpO₂ hourly for first 24 h, then 4‑hourly if stable.
- Neurological Observations: GCS, deep tendon reflexes, headache/visual changes every 4 h for 48 h
- Urine Output: Hourly monitoring; target ≥0.5 mL/kg/h.
- Fluid Balance: Strict input/output charting; cumulative balance review every 8 h.
- Laboratory: Platelets, renal/liver function, coagulation profile 6 h postoperative and daily until stable.
Pain Management
- Neuraxial Analgesia:
- Intrathecal morphine 50–100 µg for spinal; epidural morphine 2–3 mg.
- Monitor sedation and respiratory rate hourly for 12 h.
- Systemic Analgesia:
- Paracetamol 1 g QDS.
- NSAIDs (ibuprofen 400 mg QDS or ketorolac 15 mg IV Q6h) if BP <140/90 mmHg and renal function normal.
- Opioids: Oxycodone 5–10 mg PO Q4–6h PRN; avoid tramadol in seizure history.
- Regional Blocks:
- TAP or QL block with ropivacaine 0.2% 20 mL each side for additional analgesia.
Postoperative Hypertension Management
- Antihypertensives: Continue labetalol or nifedipine targeting DBP <85 mmHg.
- Monitoring: BP every 4 h for 72 h, then twice daily until discharge.
- Oral Therapy Transition: Switch to oral labetalol 100–200 mg TDS or nifedipine SR 30–60 mg OD as patient tolerates.
Fluid Management and Oliguria
- Fluid Restriction: Limit to 1 000 mL IV fluids over 24 h; allow clear fluids orally.
- Oliguria (<0.5 mL/kg/h):
- Exclude hypovolaemia, AKI, pulmonary oedema.
- If pulmonary oedema risk high, avoid bolus; consider furosemide 20 mg IV
- Diuresis Goal: Maintain euvolaemia; avoid precipitous fluid shifts.
Thromboprophylaxis
- Mechanical: Thromboembolism stockings + intermittent pneumatic compression on arrival.
- Pharmacologic:
- Enoxaparin 40 mg SC OD ≥12 h post neuraxial block or ≥4 h after catheter removal.
- Increase to 40 mg BD if BMI >40 kg/m² or weight >120 kg.
- Duration: At least 7 days; extend to 6 weeks if additional VTE risk factors.
Breastfeeding and Medication Safety
- Safe Agents: Labetalol, nifedipine, methyldopa, enalapril—compatible with breastfeeding.
- Avoid: Atenolol (bradycardia risk in infant), ACEi with high milk transfer.
- Resources: Refer to LactMed for up‑to‑date compatibility.
Mental Health and Well‑being
- Screening: Use Edinburgh Postnatal Depression Scale (EPDS) and anxiety inventories before discharge.
- Support: Trauma‑informed care; involve partner or support person; offer counselling referrals.
- Follow‑Up: Arrange mental health review at 6 weeks postpartum.
Postpartum Follow‑Up
- Cardiovascular: Clinic at 6–12 weeks for BP, renal function, lipid profile and glucose tolerance test.
- Long‑Term Risk Counselling: Advise on cardiovascular risk reduction (diet, exercise, smoking cessation).
- Family Planning: Discuss optimal interpregnancy interval and prophylactic aspirin in future pregnancies.
4th Trimester
- The “fourth trimester” (birth → 12 weeks) is the danger zone where up to 60 % of maternal deaths from hypertensive disorders occur; blood-pressure can spike or present de novo, magnesium levels fall, airway and pulmonary oedema may persist, and analgesic/antihypertensive choices still shape maternal outcomes. Anaesthetists must therefore keep treating the parturient with pre-eclampsia as “high-risk” even after placental delivery
Persistent Pathophysiology
| Issue | Why it matters in weeks 0-12 | Practical actions |
|---|---|---|
| Hypertension & end-organ risk | New-onset or rebound hypertension peaks days 3-6 postpartum and can trigger stroke, HELLP, pulmonary oedema. | Continue in-hospital BP checks ≥72 h; home monitoring until 7 days; treat ≥150/100 mm Hg with labetalol, nifedipine or hydralazine as inpatient. |
| Seizure threat | Eclamptic fits reported up to 6 weeks after delivery. | Maintain MgSO₄ for ≥24 h after last seizure or delivery; give rescue diazepam/lorazepam if seizures recur. |
| Airway and laryngeal oedema | Edema and difficult laryngoscopy can linger 48 h+ postpartum. | If GA needed (e.g., uterine curettage), use smaller ETT, ramped position; keep difficult-airway devices ready. |
| Autotransfusion & fluid shifts | Uterine involution returns 500–800 mL to circulation, risking flash pulmonary oedema in stiff LV. | Restrict crystalloids, give low-dose furosemide if symptomatic; avoid ergometrine in severe HTN. |
| Thrombocytopenia / coagulopathy | Platelets may remain < 100 × 10⁹ L⁻¹ for days | Safe neuraxial if platelets ≥ 70 × 10⁹ L⁻¹, normal coagulation and no trend down; otherwise delay or use GA with airway plan above. |
| Analgesia & NSAIDs debate | NSAIDs can raise BP but recent RCTs show ibuprofen non-inferior to paracetamol for BP control, though data are mixed. | Prefer paracetamol ± opioid until BP controlled; if using NSAID, monitor BP q4 h; avoid if platelets < 100 or creatinine ↑. |
Anaesthetic Considerations for Common Postpartum Procedures
Neuraxial Techniques
- Tubal ligation or curettage: Offer spinal (≤ 8 mg bupivacaine + opioid) to blunt hypertensive surges and avoid airway concerns; confirm platelets first.
- Epidural blood patch: Possible if platelets stable and BP controlled; rule out PRES before treating “headache.”
General Anaesthesia
- Induction: Propofol/etomidate + remifentanil or short-acting opioid to blunt pressor response; have nitroglycerin ready for severe surges.
- Extubation: Fully awake, head-up, consider IV labetalol 10 mg or nicardipine infusion to smooth emergence.
Post-discharge Safety Net
- Give the patient and family a “red flag” list: severe headache, visual change, epigastric pain, SOB.
- Arrange a BP check within 7 days and again at 6 weeks.
- Communicate anaesthetic course and any airway/platelet issues to primary-care team for future pregnancies.
Links
- Hypertension
- Obstetric haemorrhage
- Obstetric emergencies
- Obstetric physiology
- Amniotic fluid embolism and PE
- Stroke
Past Exam Questions
Anaesthetic Considerations in a Parturient with Severe Hypertension
A 25-year-old parturient at term in her third pregnancy presents with a blood pressure of 155/115 mmHg.
a) What other parameters are required to make a diagnosis of pre-eclampsia? (5)
The parturient goes into labour overnight and presents for a caesarean section.
b) What features on pre-operative evaluation would make you consider general rather than neuraxial anaesthesia? (5)
Test You Knowledge
- Define preeclampsia and list the two key diagnostic criteria required after 20 weeks’ gestation.
- Compare and contrast chronic hypertension, gestational hypertension and preeclampsia in terms of timing, proteinuria and end-organ dysfunction.
- Describe four severe features of preeclampsia and give the threshold values or findings for each.
- Outline the two-stage model of preeclampsia pathophysiology, naming the placental abnormality and the circulating factors involved.
- List five acute maternal complications of preeclampsia and briefly explain the mechanism or consequence of each.
- Explain your anaesthetic plan for a patient with severe preeclampsia and a platelet count of 80 × 10⁹/L who requires an emergency caesarean section.
- Discuss the fluid management strategy in preeclampsia, including how and why you would use invasive monitoring to guide therapy.
- Describe the regimen for seizure prophylaxis in preeclampsia, including dosing and duration.
- Identify three echocardiographic findings you would look for in a preeclamptic patient with suspected HFpEF, and name the relevant biomarker thresholds.
- Compare the intraoperative anaesthetic choices (neuraxial vs general) in preeclampsia, giving at least two indications and two contraindications for each.
- Outline your postoperative thromboprophylaxis plan, including timing relative to neuraxial blockade and duration.
- Summarise the key elements of postpartum follow-up for cardiovascular risk reduction after a preeclamptic pregnancy.
References:
- Melchiorre K, et al. Cardiovascular function in women with a history of early onset preeclampsia. Hypertension. 2020;75(4):1128–1136.
- McDonald SD, Malinowski A. Long-term hypertension post preeclampsia. BJOG. 2019;126(3):338–347.
- Wu P, et al. Long-term risk of cardiovascular disease in women with preeclampsia. JAMA Cardiol. 2017;2(8):778–785.
- Proudfoot NR, et al. Neurocognitive sequelae of preeclampsia. Am J Obstet Gynecol. 2021;225(1):110.e1–110.e12.
- Rolnik DL, et al. Aspirin versus placebo in pregnancies at high risk for preterm preeclampsia. N Engl J Med. 2017;377(7):613–622.
- Hofmeyr GJ, et al. Calcium supplementation to prevent preeclampsia: meta-analysis. BJOG. 2014;121(10):1181–1190.
- National Institute for Health and Care Excellence. Hypertension in pregnancy: diagnosis and management. CG132. 2020.
- Royal College of Obstetricians and Gynaecologists. Postpartum care. Green-top Guideline No.37. 2018.
- American College of Obstetricians and Gynecologists. Practice Bulletin No.207: Thromboembolism in pregnancy. Obstet Gynecol. 2020;135(2):e1–e13.
- Moore D, ed. Drugs in Lactation. Larvol. 2023.
- Howard LM, et al. Perinatal mental health. Lancet. 2014;384(9956):1775–1788
- Dyk, D. v., Dyer, R. A., & Fernandes, N. (2021). Preeclampsia in 2021—a perioperative medical challenge for the anesthesiologist. Anesthesiology Clinics, 39(4), 711-725. https://doi.org/10.1016/j.anclin.2021.08.005
- POLLEY, LINDA S. MD. Anesthetic Management of Hypertension in Pregnancy. Clinical Obstetrics and Gynecology 46(3):p 688-699, September 2003.
- Sharma DD, Chandresh NR, Javed A, Girgis P, Zeeshan M, Fatima SS, Arab TT, Gopidasan S, Daddala VC, Vaghasiya KV, Soofia A, Mylavarapu M. The Management of Preeclampsia: A Comprehensive Review of Current Practices and Future Directions. Cureus. 2024 Jan 2;16(1):e51512. doi: 10.7759/cureus.51512. PMID: 38304688; PMCID: PMC10832549.
- Seymour, Lisa M. MBChB; Fernandes, Nicole L. FCA(SA); Dyer, Robert A. FCA(SA), PhD,†; Smit, Maretha I. FCA(SA); van Dyk, Dominique FCA(SA); Hofmeyr, Ross FCA(SA), FAWM. General Anesthesia for Cesarean Delivery for Thrombocytopenia in Hypertensive Disorders of Pregnancy: Findings From the Obstetric Airway Management Registry. Anesthesia & Analgesia 136(5):p 992-998, May 2023. | DOI: 10.1213/And.0000000000006217
- FRCA Mind Maps. (2024). Retrieved June 5, 2024, from https://www.frcamindmaps.org/
- Anesthesia Considerations. (2024). Retrieved June 5, 2024, from https://www.anesthesiaconsiderations.com/
- The Calgary Guide to Understanding Disease. (2024). Retrieved June 5, 2024, from https://calgaryguide.ucalgary.ca/
Summaries
[PET
MGS04
PET Calgary guide
Copyright
© 2025 Francois Uys. All Rights Reserved.
id: “20de9629-1011-464d-92ef-07c1abde548d”



