{}
Summary
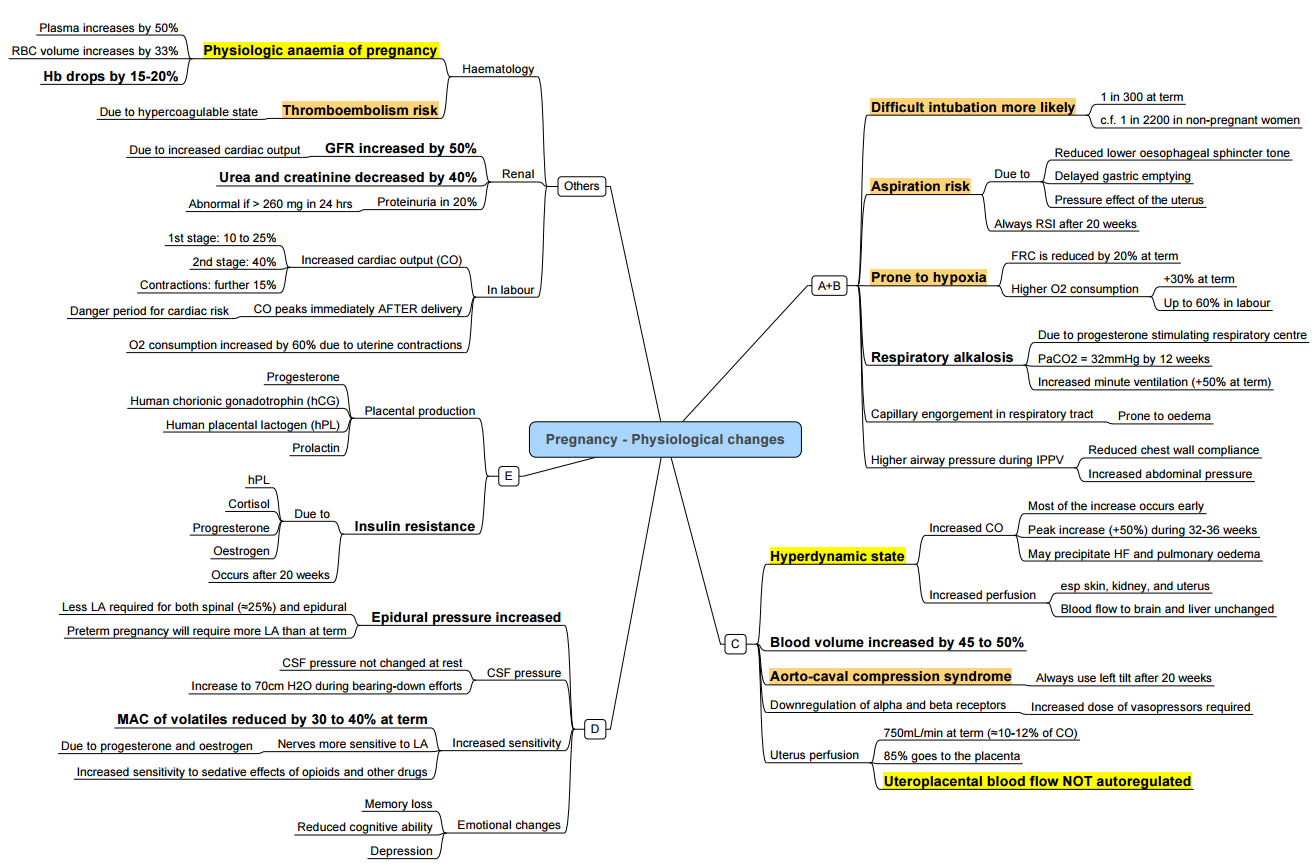
Physiological Changes in Pregnancy
Cardiovascular System (CVS)
- Intravascular volume increases by 35–45%; plasma volume by 40–50%; erythrocyte mass by 20–30%, resulting in physiological anaemia (haemodilution).
- Total blood volume reaches 90 mL/kg.
- Cardiac output ↑ 40–50% (↑ stroke volume 25–30%; ↑ heart rate 15–25%).
- Systemic vascular resistance ↓ ~20%; pulmonary vascular resistance ↓ ~35%.
- Central venous pressure and pulmonary capillary wedge pressure remain unchanged; femoral venous pressure ↑ ~15%.
- Aortocaval compression: supine hypotension syndrome in 8–10% of women (↓ mean arterial pressure > 15 mmHg, ↑ heart rate > 20 bpm) due to gravid uterus compressing the inferior vena cava—left lateral tilt is recommended from mid-second trimester onwards.
- Electrocardiogram: slight rightward QRS axis shift in first trimester, leftward in third; minor ST-segment depression and T-wave flattening in lateral leads.
- Echocardiography: 10–20% enlargement of cardiac chambers (predominantly right heart), eccentric left ventricular hypertrophy, trivial regurgitation across atrioventricular valves, occasional small pericardial effusion.
Respiratory Changes
- Minute ventilation ↑ 40–50% (↑ tidal volume 40–45%; respiratory rate ↑ 5–15%), leading to respiratory alkalosis (arterial pH ~ 7.44, PaCO₂ ~ 30 mmHg, HCO₃⁻ ~ 20 mmol/L).
- Functional residual capacity ↓ 20%; expiratory reserve volume ↓ 20–25%; residual volume ↓ 15–20%, with minimal change in total lung capacity.
- Oxygen consumption ↑ 20–35% at term; further ↑ during labour (1st stage + 40%, 2nd stage + 75%).
- Airway mucosa is oedematous and hyperaemic, increasing risk of bleeding during instrumentation; breast enlargement and weight gain may complicate airway management.
Airway Changes
- Capillary engorgement increases risk for trauma and bleeding.
- Enlarged breast size can complicate laryngoscopy.
Neurological Changes
- MAC: Decreased 40% due to progesterone effects and beta-endorphin levels (sedative effect).
- Local Anaesthetics: Decrease dose by 30%. Hormonal effects and engorgement of the epidural venous plexus lead to decreased spinal cerebrospinal fluid volume, decreased epidural space volume, and increased epidural pressure.
Renal Changes
- Glomerular filtration rate ↑ ~ 50%, with corresponding ↓ serum creatinine (to ~ 0.4–0.6 mg/dL) and urea.
- Plasma osmolality ↓ by 8–10 mOsm/kg; thirst threshold lowered.
Coagulation Changes
- Haemoglobin concentration ↓ ~ 12–14 g/dL; white cell count ↑ up to 15 × 10⁹/L; platelet count may fall by 10–20%.
- Coagulation: ↑ fibrinogen (factor I), factors VII, VIII, IX, X, XII and von Willebrand factor; ↓ antithrombin III and protein S; net hypercoagulable state reduces bleeding risk but ↑ thromboembolism.
Gastrointestinal Changes
- Increased gastroesophageal reflux and esophagitis.
- Reduced gastric motility and incompetence of gastroesophageal sphincter due to uterine displacement.
- 30%-60% of pregnant patients have a gastric volume >25 mL or gastric fluid pH <2.5.
- High risk for regurgitation and pulmonary aspiration.
Hepatic Changes
- Decreased pseudocholinesterase by 30%.
- High progesterone levels inhibit cholecystokinin release, leading to incomplete gallbladder emptying and gallstones.
- Minor elevations in AST, ALT, ALP, and LDH.
- Plasma protein concentrations decrease: 25% decrease in albumin, 10% decrease in total protein at term.
- Colloid osmotic pressure decreases from 27 to 22 mmHg during gestation.
Metabolic Changes
- Diabetogenic state with increased insulin levels due to human placental lactogen leading to insulin resistance.
- Pancreatic beta cell hyperplasia in response to increased insulin demand.
- Elevated levels of thyroxine (T4) and triiodothyronine (T3) due to increased thyroid-binding globulin; free T4, free T3, and TSH remain normal.
- Serum calcium levels decrease, but ionized calcium concentration remains normal.
Musculoskeletal Changes
- Increased relaxin leading to backache.
Endocrine Changes
- Placenta Produces:
- Progesterone
- Estrogen
- Prostaglandins
- Human placental lactogen (HPL)
- Human chorionic gonadotropin (HCG)
- Pituitary:
- Increased ACTH and prolactin.
- RAAS Stimulation:
- Directly by estrogen.
- Indirectly by progesterone’s natriuretic effect reducing sodium and stimulating RAAS.
- Adrenals:
- Increased cortisol.
- Thyroid:
- Increased T3, T4, and thyroxine-binding globulin; normal unbound levels.
- Pancreas:
- Increased insulin secretion with reduced tissue sensitivity, leading to more glucose availability for the fetus.
Delivery
- Minute ventilation may increase up to 300%.
- Oxygen consumption increases by an additional 60% above third-trimester values.
- Excessive hyperventilation can cause PaCO2 to decrease below 20 mm Hg.
- Marked hypocapnia can lead to hypoventilation and transient maternal and fetal hypoxemia between contractions.
- Excessive hyperventilation reduces uterine blood flow and promotes fetal acidosis.
- Each contraction displaces 300-500 mL of blood from the uterus into the central circulation, increasing cardiac output by 45% over third-trimester values.
- The greatest cardiac strain occurs immediately after delivery, with cardiac output increasing up to 80% above late third-trimester values.
Return to Normal
- FRC: Returns to normal within 48 hours after delivery.
- Blood Volume: Normalizes within 1-2 weeks.
- Pseudocholinesterase Levels: Return to normal within 6 weeks.
- MAC: Returns to normal by 72 hours postpartum.
- Dosage Requirements for Regional Anesthesia: Return to normal within 24-36 hours.
- Gastric Volume and Fluid pH: Normalize within 24 hours after delivery.
- Some physiological changes may take up to 6 weeks for resolution.
- Cardiac Output: Decreases substantially toward prepregnant values by 2 weeks postpartum, with complete return to nonpregnant levels between 12 and 24 weeks postpartum.
Links
- Non obstetric surgery
- Fetus and Placenta
- Maternal conditions
- Obstetric haemorrhage
- Obstetric emergencies
References:
- Allman K, Wilson I, O’Donnell A. Oxford Handbook of Anaesthesia. Vol. 4. Great Clarendon Street, Oxford, OX2 6DP, United Kingdom: Oxford University Press; 2016. 1295 p. Allman et al. – Oxford Handbook of Anaesthesia.pdf
- Butterworth J, Mackey D, Wasnick J. Morgan and Mikhail’s Clinical Anesthesiology, 7th Edition. 7th edition. New York: McGraw Hill Medical; 2022.
- Gropper, M. A. (Ed.). (2019). Miller’s Anesthesia (9th ed.). Philadelphia, PA: Elsevier.
- Canobbio, M. M., Warnes, C. A., Aboulhosn, J., Connolly, H. M., Khanna, A., Koos, B. J., … & Stout, K. (2017). Management of pregnancy in patients with complex congenital heart disease: a scientific statement for healthcare professionals from the american heart association. Circulation, 135(8). https://doi.org/10.1161/cir.0000000000000458
- Bhatia N, Riou B. Cardiovascular physiology of pregnancy. Br J Anaesth. 2018;120(3):475–486
- Leighton BL, Smith IP. Respiratory physiology in pregnancy. Curr Opin Anaesthesiol. 2019;32(3):345–350.
- Miller RD, Cohen NH, Eriksson LI, et al., editors. Miller’s Anesthesia. 9th ed. Philadelphia: Elsevier; 2020.
- FRCA Mind Maps. (2024). Retrieved June 5, 2024, from https://www.frcamindmaps.org/
- Anesthesia Considerations. (2024). Retrieved June 5, 2024, from https://www.anesthesiaconsiderations.com/
Summaries
Obs physiology
—
Copyright
© 2025 Francois Uys. All Rights Reserved.
id: “ecb96c02-e36e-45ed-b40e-ff76851f02dd”



