{}
Cardiac Protection
Introduction
Preconditioning (PC) describes brief, non-lethal insults that render tissue more resistant to a subsequent, prolonged ischaemic event.
- Ischaemic PC–repeated coronary occlusion/reperfusion cycles before the index ischaemia.
- Anaesthetic (pharmacological) PC–volatile agents and several intravenous agents mimic ischaemic PC.
- Remote ischaemic PC (RIPC)–cycles applied to a distant tissue (e.g., limb cuff).
- Post-conditioning–brief occlusion/reperfusion applied after the index ischaemia to attenuate reperfusion injury.
Time Windows of Protection
| Window | Onset | Duration | Predominant mechanisms | Leads to protection against |
|---|---|---|---|---|
| Early | within 15 min | 2–6 h | Receptor-mediated signalling (RISK/SAFE*), K_ATP opening, mitochondrial permeability transition pore (mPTP) inhibition | Infarction (not stunning) |
| Late | 12–96 h | up to 4 d | Gene transcription (heat-shock proteins, iNOS, COX-2), anti-apoptosis | Infarction and stunning |
RISK = Reperfusion injury salvage kinase; SAFE = Survival activating factor enhancement.
Pathophysiology of Cardioprotection
- Trigger–adenosine, bradykinin, opioids, volatile agents, pacing, ischaemia.
- Transduction–activation of PKC, PI3K-Akt, JAK–STAT, ROS, nitric oxide.
- End-effector–mitochondrial K_ATP channel opening → prevents mPTP opening on reperfusion, preserves ATP, limits Ca²⁺ overload, reduces apoptosis.
- Propofol’s antioxidant action scavenges ROS but also blunts ROS-triggered signalling and may therefore inhibit both ischaemic/RIPC and volatile PC.
Modalities of pre-/post-conditioning
- Direct ischaemic conditioning: myocardial or aortic cross-clamp cycles (historical interest only).
- Remote limb conditioning: simple, inexpensive, but large RCTs (ERICCA, RIPHeart) and recent meta-analyses show no improvement in hard outcomes; benefit confined to selected paediatric cohorts without propofol.
- Volatile anaesthetic PC: most consistent clinical signal (troponin reduction, improved LV function).
- Pharmacological adjuvants: adenosine, cyclosporine, sodium-glucose cotransporter-2 inhibitors, GLP-1 analogues–evidence remains experimental/early phase.
Relevance to Anaesthesiologists
Choice of Maintenance Agent
| Evidence 2017–2025 | Key findings | Clinical message |
|---|---|---|
| MYRIAD RCT (5 395 CABG pts) | Volatile vs propofol–no difference in 1-y mortality or MI | Volatiles not mandated purely for survival benefit |
| 2020–2024 meta-analyses | Volatiles ↓ peak cTn and CK-MB, modest ↓ ICU stay; long-term mortality signal heterogeneous | Volatiles reasonable when myocardial protection prioritised |
| 2023 OPCAB meta-analysis | Sevoflurane superior to propofol for troponin release; no mortality difference | Supports volatile use in off-pump grafting |
| Propofol interaction | Propofol infusion (≥2 mg kg⁻¹ h⁻¹) abolishes volatile and RIPC benefits in several subgroup analyses | If propofol required, minimise dose or avoid RIPC protocols |
Current 2024 EACTS/EACTAIC guidelines do not recommend any anaesthetic solely for cardioprotection. Agent choice should be individualised and haemodynamic goals prioritised.
Practical Peri-operative Measures
- Maintain normothermia, normoglycaemia, adequate haemoglobin and coronary perfusion pressure.
- Avoid tachycardia, severe hypotension and prolonged aortic cross-clamp time.
- Consider low-dose volatile (0.5–1 MAC) before and immediately after CPB if haemodynamics allow.
- Limit high-dose propofol infusions when employing RIPC or seeking volatile PC benefit.
- Early weaning, lung-protective ventilation and multimodal opioid-sparing analgesia complement myocardial protection.
Propofol versus Volatile agents–summary
| Aspect | Propofol | Volatiles (sevoflurane/desflurane) |
|---|---|---|
| Antioxidant / ROS scavenger | ✔︎ (direct) | Mild, indirect |
| Triggers RISK/SAFE pathways | ✖︎ (may inhibit) | ✔︎ |
| Haemodynamic stability | Predictable ↓ SVR | Dose-dependent myocardial depression |
| Evidence for ↓ troponin | Mixed | Consistent ↓ (~15–30 %) |
| Long-term mortality | Neutral; meta-analysis signals possible ↑ in high-risk subsets | Neutral overall; possible ↓ in CPB cohorts |
| Interference with RIPC | Inhibits | Nil |
- Clinical take-away: In patients with limited ischaemic burden or when TIVA provides other advantages (e.g., neurological monitoring, malignant hyperthermia risk), propofol remains appropriate. Where myocardial tolerance to ischaemia is paramount (poor left ventricular function, long cross-clamp), a volatile-based technique (with low propofol doses, if any) is rational.
Modalities of Preconditioning
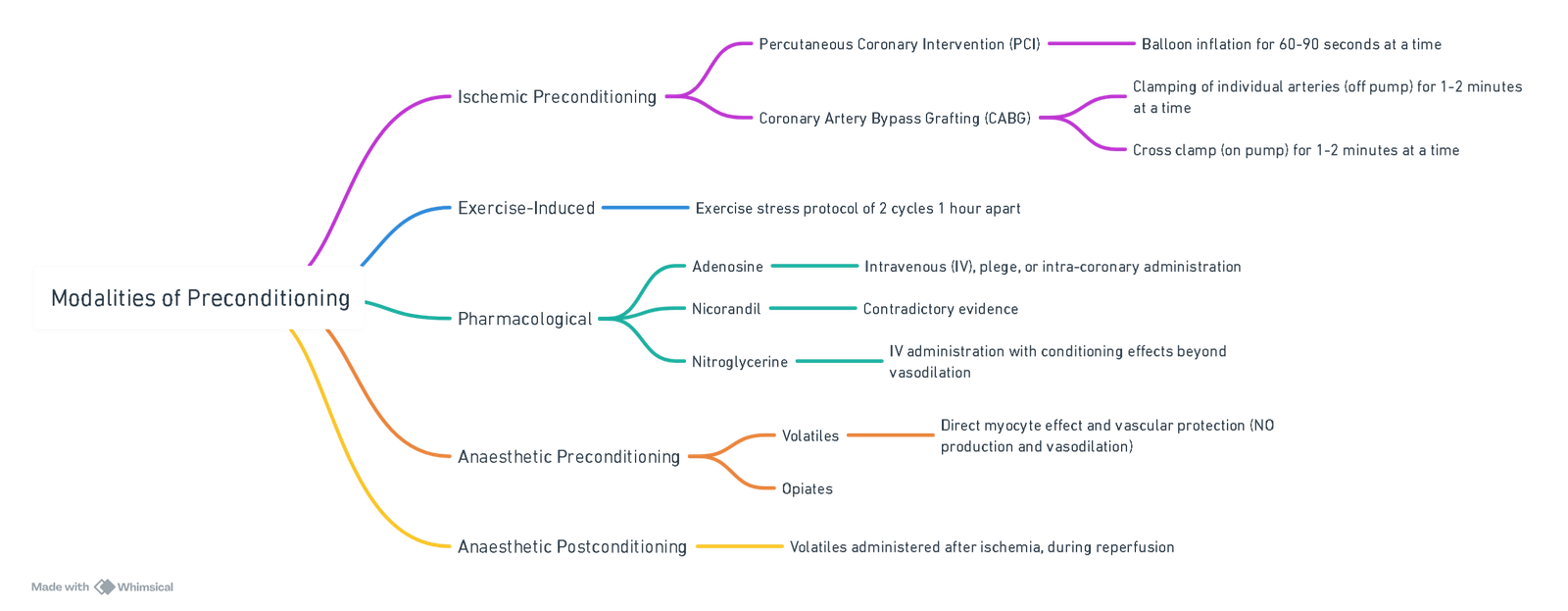
View or edit this diagram in Whimsical.
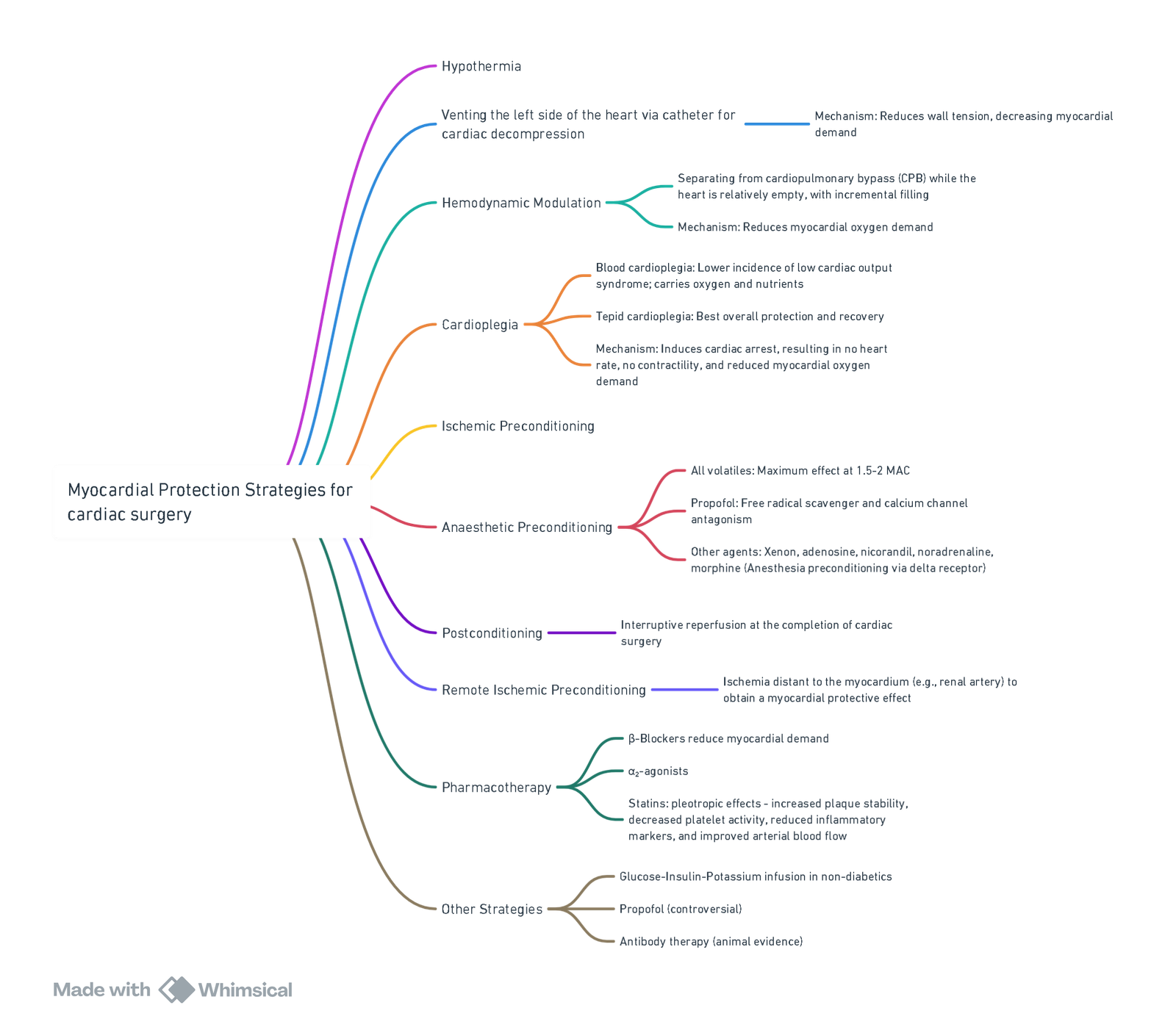
Cardiac Surgery
Non-Cardiac Surgery
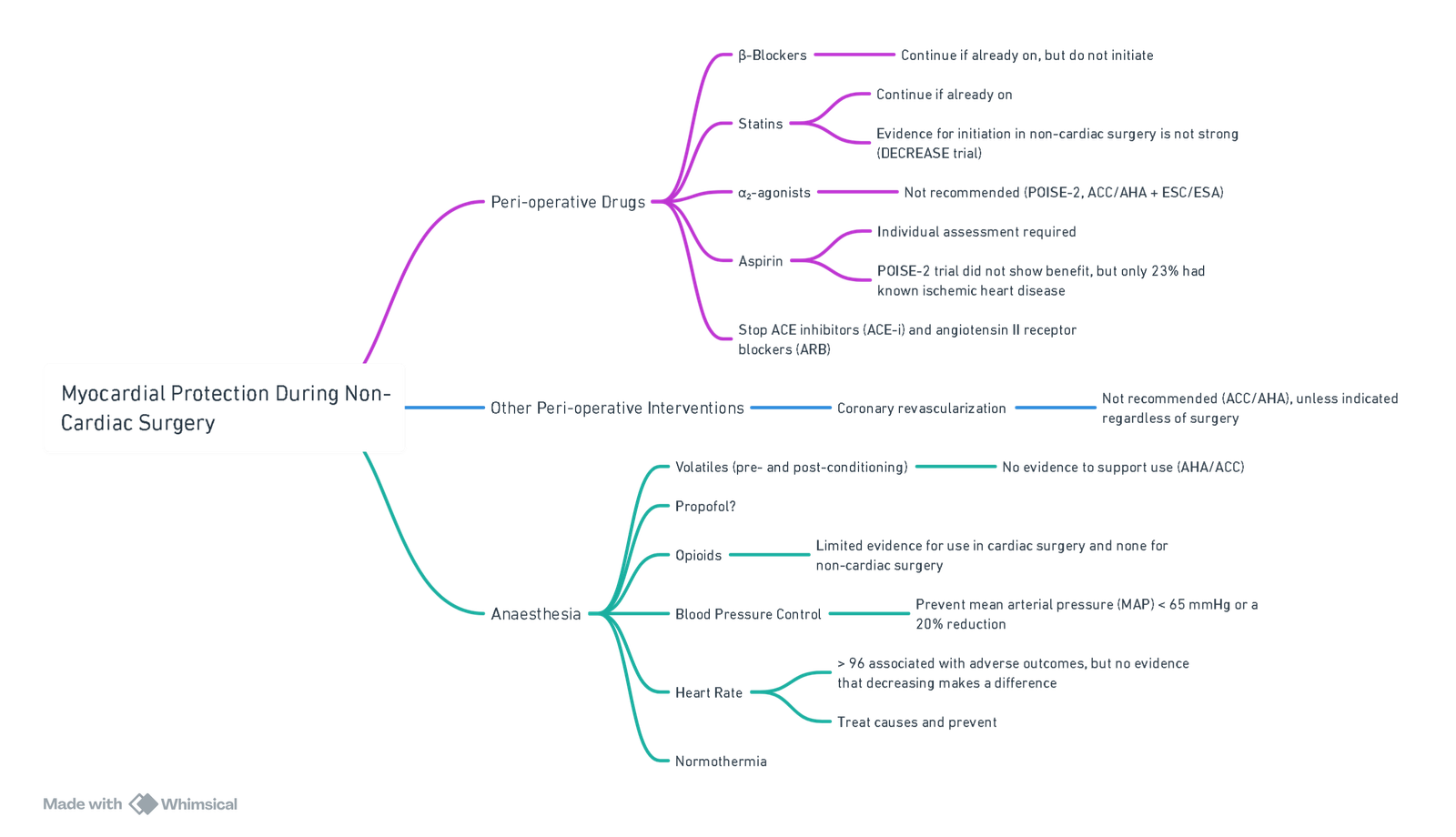
View or edit this diagram in Whimsical.
NB: All the above apply to non-cardiac surgery only!
*POISE-3 is investigating whether a MAP cutoff of 80 mmHg is superior to 65 mmHg.
Links
- Cardiac physiology
- Peripheral Vascular Disease (PVD) and Risk Stratification
- Ischaemic heart disease
- Coronary artery bypass surgery (CABG)
- Off Pump CABG
- Cath lab anaesthesia
- Organ protection
Past Exam Questions
Myocardial Protective Measures in Cardiac Surgery
List myocardial protective measures that can be used during cardiac surgery. (10)
References:
- Wong, S.S.C. and Irwin, M.G. (2016), Peri-operative cardiac protection for non-cardiac surgery. Anaesthesia, 71: 29-39. https://doi.org/10.1111/anae.13305
- Zhang C, He C, Chen Z, et al. The effects of volatile anesthetics and propofol in patients undergoing off-pump coronary artery bypass grafting: a systematic review and meta-analysis. Front Cardiovasc Med. 2023;10:1271557. Available from: https://pubmed.ncbi.nlm.nih.gov/38034375 pmc.ncbi.nlm.nih.gov
- Landoni G, Lomivorotov VV, Alvaro G, et al. Volatile Anesthetics versus Total Intravenous Anesthesia for Cardiac Surgery (MYRIAD trial). N Engl J Med. 2019;380:1214-25. Available from: https://pubmed.ncbi.nlm.nih.gov/30888743 pubmed.ncbi.nlm.nih.gov
- Wahba A, Kunst G, De Somer F, et al. 2024 EACTS/EACTAIC/EBCP Guidelines on cardiopulmonary bypass in adult cardiac surgery. Br J Anaesth. 2025;134:917-1008. Available from: https://pubmed.ncbi.nlm.nih.gov/ PMCID: PMC11947607 pmc.ncbi.nlm.nih.gov
- Li J, Wang X, Wu S, et al. Remote ischaemic preconditioning and clinical outcomes after paediatric cardiac surgery: systematic review and meta-analysis. BMC Anesthesiol. 2023;23:112. Available from: https://pubmed.ncbi.nlm.nih.gov/37005591 pmc.ncbi.nlm.nih.gov
- Hausenloy DJ, Candilio L, Evans R, et al. Remote ischaemic preconditioning and outcomes of cardiac surgery (ERICCA trial). N Engl J Med. 2015;373:1408-17. Available from: https://pubmed.ncbi.nlm.nih.gov/26436207 nejm.org
- Bonanni A, Signori A, Alicino C, et al. Volatile anesthetics versus propofol for cardiac surgery with cardiopulmonary bypass: meta-analysis of randomised trials. Anesthesiology. 2020;132:1429-46. Available from: https://europepmc.org/article/med/32205551 europepmc.org
- FRCA Mind Maps. (2024). Retrieved June 5, 2024, from https://www.frcamindmaps.org/
- Anesthesia Considerations. (2024). Retrieved June 5, 2024, from https://www.anesthesiaconsiderations.com/
Summaries:
Myocardial protection
Copyright
© 2025 Francois Uys. All Rights Reserved.
id: “8e585a50-20c3-4f2c-b177-2fdc593f5c54”



