- Upper Limb Block
- Nerve Injury After Peripheral Nerve Block–Recognition & Evidence-Based Pathway
- Links
{}
Upper Limb Block
Overview
- The entire upper limb (shoulder → hand) is supplied by the Brachial plexus (C5–T1).
- Regional techniques are chosen according to:
- Surgical field & tourniquet site
- Need for diaphragm-sparing (respiratory comorbidity, obesity, pregnancy)
- Post-operative analgesia duration (single-shot vs catheter)
- Available imaging (ultrasound is standard of care)
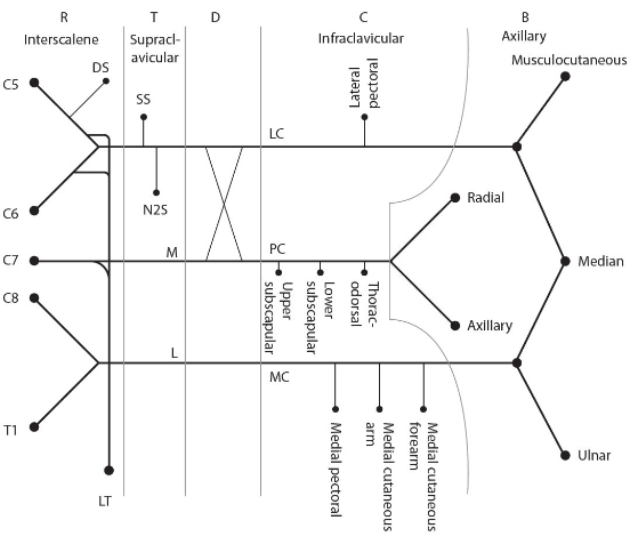
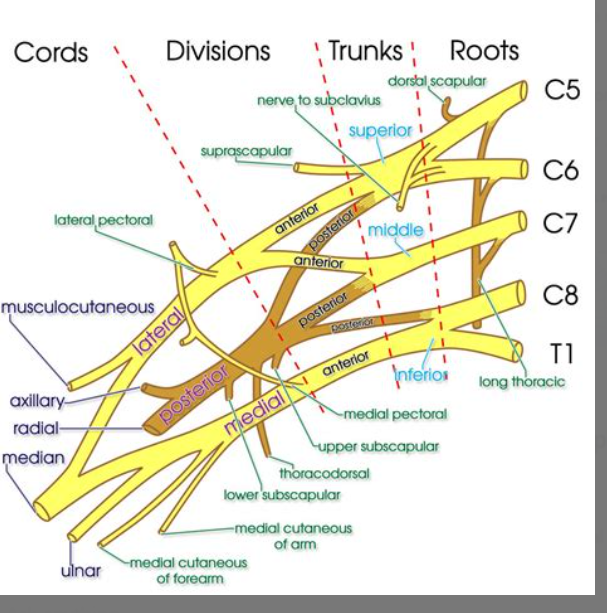
Brachial Plexus
| Level | Components | Main relations & landmarks | Key motor/sensory targets |
|---|---|---|---|
| Roots (ventral rami) | C5–T1 (± C4, T2 variants) | Emerge between anterior & middle scalene muscles in the posterior cervical triangle; run with the subclavian artery | Segmental branches: dorsal scapular (C5), long thoracic (C5–7), to scalene & longus colli |
| Trunks | Superior (C5-6), Middle (C7), Inferior (C8-T1) | Lie superior & posterior to the subclavian artery at the lateral border of the scalene muscles, directly above the first rib | Suprascapular & nerve to subclavius (from superior trunk) |
| Divisions | Each trunk splits into anterior & posterior divisions posterior to the clavicle | Pass deep to the clavicle and pectoralis minor with the second part of the axillary artery | No named branches |
| Cords | Fusion of divisions around the axillary artery in the axilla—lateral, posterior, medial (named by position to artery) | Deep to pectoralis minor, envelop the axillary artery | Lateral & medial pectoral, thoracodorsal, subscapulars, medial cutaneous nerves of arm/forearm |
| Terminal branches | Musculocutaneous (C5-7), Axillary (C5-6), Radial (C5-T1), Median (C5-T1), Ulnar (C8-T1) | Exit axilla at the inferior border of teres major & through the cubital fossa/arm | Motor & cutaneous supply to the entire upper limb except trapezius (cranial XI) & small medial upper-arm area (T2 intercostobrachial) |
- Summary only; many smaller muscular & cutaneous branches arise proximally.
Organisational Mnemonics
- “Randy Travis Drinks Cold Beer” → Roots → Trunks → Divisions → Cords → Branches.
Clinical Pearls (anaesthetic relevance)
- Block approach aligns with levels: interscalene (roots/trunks), supraclavicular (trunks/divisions), infraclavicular (cords), axillary (terminal branches).
- Phrenic nerve risk highest with interscalene block (C3-5 proximity).
- Vascular neighbours: Subclavian/axillary artery is the constant landmark; cords wrap around it—posterior cord posterior, etc.
- Common injury sites: Erb’s point (upper trunk traction → C5-6 palsy); Klumpke (lower trunk traction); posterior cord compression (crutch palsy).
Different Blocks
| Approach (US-guided) | Plexus level | Usual LA volume | Typical operations | Tourniquet cover | Specific complications (incidence) | Key caveats | Landmark (US probe position) | Needle technique | Motor-/sensory nerve-stim end-point |
|---|---|---|---|---|---|---|---|---|---|
| Interscalene (ISB) | Roots C5–C7 | 10–15 mL | Shoulder arthroplasty, proximal humerus fixation | Poor (upper arm) | Phrenic-nerve palsy (80–100 %), Horner’s (~20 %), RLN block (~10 %) | Avoid in severe COPD / contralat. hemidiaphragm palsy | Linear probe transverse at C6 (cricoid) over interscalene groove between anterior & middle scalene | In-plane lateral-to-medial; inject around visible root cluster | Deltoid / biceps twitch < 0.5 mA (or no twitch with pure US) |
| Supraclavicular (SCB) | Trunks / divisions | 15–25 mL | Arm, elbow, radial-forearm | Excellent | Pneumothorax (0–0.7 %), Horner’s (~30 %), vascular puncture (~3 %) | Pleural proximity ↓ with US | Probe parallel to clavicle, medial to mid-clavicle, plexus “grapes” posterolateral to subclavian artery | In-plane lateral-to-medial; circumferential spread around trunks | Finger / wrist flex-ext twitch < 0.5 mA |
| Infraclavicular (ICB) | Cords | 20–30 mL | Elbow, forearm, hand | Excellent | Axillary/subclavian vessel puncture (4–10 %), pneumothorax (<0.2 %) | Deeper; heed anticoagulation | Probe parasagittal below clavicle, medial to coracoid; cords around axillary artery/vein | In-plane cephalad-to-caudad; stalk needle into posterior cord first | Hand extension/supination or biceps twitch < 0.5 mA |
| Axillary | Terminal branches | 20–30 mL | Hand, wrist | Good | Incomplete block (missed MCN) (5–20 %), vascular puncture (2–9 %) | Block musculocutaneous separately | Probe high axilla, visualize axillary artery with radial, median, ulnar around; MCN between coraco- & biceps | Multiple in-plane injections around each nerve; MCN blocked separately in coracobrachialis | Individual nerve twitches: thumb flex (median), 5th finger flex (ulnar), wrist/finger ext (radial), biceps (MCN) < 0.5 mA |
| Distal single-nerve (median, ulnar, radial, MCN) | Individual nerves | 3–5 mL | Wrist / hand | None | Incomplete sensory block (~2 %), transient neuritis (<0.1 %) | Preserves proximal motor | Probe over target nerve at elbow/forearm | In-plane or out-of-plane; inject sheath | Appropriate distal motor response (e.g. thumb opposition for median) < 0.5 mA |
| IVRA (Bier) | Intravenous | 0.5 % Prilocaine 3 mg kg⁻¹ (≤ 400 mg) | Short forearm / hand (< 60 min) | Tourniquet only | Tourniquet pain (~20 %), systemic toxicity if cuff premature (<0.1 %) | ≥ 30 min cuff; no adrenaline | IV cannula dorsum of hand; double-cuff tourniquet upper arm | Exsanguination → inject LA IV under cuff | Not applicable–nerve stim not used |
Phrenic Nerve Sparing Blocks
- When a patient’s respiratory reserve is limited, replacing ISB with either a superior trunk block or a combined suprascapular + axillary block preserves shoulder analgesia yet dramatically lowers the risk of diaphragmatic dysfunction.
- STB is a single-needle, fast option that mimics ISB onset and duration; the dual-nerve strategy is slightly more time-consuming but virtually eliminates phrenic involvement.
Why Phrenic-sparing Blocks Matter
- A conventional interscalene brachial plexus block (ISB) anaesthetises the C5–C7 roots that lie <2 mm from the phrenic nerve; even with ultrasound and low volumes, ≈70–100 % of patients develop hemidiaphragmatic paresis, cutting FVC by 20-30 %. In healthy people that is tolerated, but in COPD, obesity, pregnancy, severe asthma or contralateral lung pathology it can precipitate hypoxaemia or hypercapnia.
Phrenic-sparing Alternatives for Shoulder Surgery
| Block | Technical note | Analgesic efficacy vs ISB | Incidence of hemi-diaphragmatic paresis |
|---|---|---|---|
| Superior trunk block (STB) | 5–10 mL LA deposited around the fused C5-C6 trunk just above the subclavian artery | RCTs & 2023 meta-analysis: equal pain scores, opioid use and PACU discharge times | 0–15 % (≈ 80 % relative risk reduction) |
| Suprascapular + axillary nerve block (SSNB + ANB) | 8–10 mL around suprascapular nerve in suprascapular or supraclavicular fossa plus 5–8 mL around axillary nerve in the quadrilateral space | Large RCTs 2020–2024 show non-inferior 24 h pain and opioid consumption; sometimes need supplemental LA to skin portals | < 5 %; often zero when ultrasound-guided |
Mechanism of Diaphragm Sparing
- Both techniques target sensory supply to the glenohumeral joint distal to the phrenic nerve’s course.
- The superior trunk injection sits caudal-posterior to the nerve, limiting cephalad spread, while the separate SSNB + ANB approach omits the root/trunk region entirely. Hence the phrenic nerve usually remains outside the LA field.
General Complications Common to all Upper-limb Blocks
- Local anaesthetic systemic toxicity (LAST)
- Infection (skin / deep tissue)
- Nerve injury (transient or permanent)
- Vascular injury or haematoma
- Block failure
- Anaphylaxis
Tourniquet Pain
Pathophysiology
- Ischaemia & nerve fibre imbalance–prolonged cuff inflation produces distal tissue ischaemia. Unmyelinated C-fibres (slow, dull pain) become progressively activated while myelinated A-δ fibres (fast pain/pressure) are blocked by local anaesthetic; loss of A-δ–mediated “gate control” unmasks C-fibre discharge.
- Metabolic mediators–local acidosis, potassium and bradykinin sensitise nociceptors.
- Sympathetic contribution–afferent sympathetic fibres may transmit pain and drive tourniquet-induced hypertension.
Typical Onset & Course
| Limb | Mean onset after inflation | Haemodynamic correlate |
|---|---|---|
| Upper | 25–35 min | HR & MAP rise ≈ 15 % from baseline |
| Lower | 35–45 min | Similar but more gradual |
- Pain intensifies until cuff deflation and can outlast block sensory level.
Prevention & Management Options
| Strategy (level of evidence) | Key details | Outcome benefit |
|---|---|---|
| Double-cuff technique (expert opinion) | Inflate distal cuff after 30 min, deflate proximal cuff | Delays pain by additional 15–20 min; standard in IV |
| Lower cuff pressure / limb exsanguination (observational) | Pressure 100 mmHg above systolic (upper limb) or < 250 mmHg | ↓ incidence & intensity of pain; fewer haemodynamic sur |
| Adjuvants to IVRA | ||
| 1. | Dexmedetomidine 0.25–0.5 µg kg⁻¹ added to lidocaine (RCT 2023) | Prolongs tourniquet tolerance by ≈ 18 min; ↓ intra-op opioids |
| 2. | Ketamine 0.3 mg kg⁻¹ IV or 0.1 mg kg⁻¹ in IVRA (RCTs 2001–2019) | Prevents tourniquet-induced hypertension; pain scores |
| 3. | Clonidine 1 µg kg⁻¹ in IVRA (meta-analysis 2022) | Extends analgesia 12 min |
| Intercostobrachial (T2) field block (2 RCTs 2022–2023 ± small RCTs 2018; cadaver / observational anatomy studies) |
1–3 mL 1–1.5 % lidocaine (or 0.25 % ropivacaine) infiltrated subcutaneously along the posterior axillary fold or ultrasound-guided injection between serratus anterior & intercostal muscles at 2nd rib to envelop the intercostobrachial nerve. • Performed after brachial-plexus block, before tourniquet inflation. • Pure sensory nerve → no motor impairement. |
• Pain-score reduction: mean NRS ↓ ~3–4 points vs control and 60 % fall in opioid rescue use; onset of discomfort delayed ≈15–20 min during 200–250 mmHg cuffs • No haemodynamic surges in ≥90 min tourniquet times (small RCT). • A second RCT with dense supraclavicular blocks found no statistically significant advantage, suggesting benefit may be greatest when the proximal block does not spread to T2 or when ≥60 min inflation is anticipated. |
| Systemic analgesia (randomised data) | Fentanyl 1 µg kg⁻¹ or remifentanil 0.05 µg kg⁻¹ min⁻¹ infusion started at 20 min | Blunts HR/MAP rise; patient |
| Rescue during block | Incremental propofol or midazolam + short-acting opioid; if pain uncontrolled after 60 min consider cuff deflation–re-inflation (“deflate-reperfuse-re-inflate”) or convert to GA | Prevents catecholamine surge an |
| Post-deflation care | Observe ≥ 20 min for rebound hypotension, LAST from IVRA | Early mobilisation once sensat |
Adjuvants & Catheters
| Adjuvant | Dose (perineural) | Benefit | Caveats |
|---|---|---|---|
| Dexamethasone | 4 mg | ↑ block duration 6–10 h; ↓ PONV | Hyperglycaemia, avoid infection focus |
| Dexmedetomidine | 25–50 µg | ↑ duration ≈ dexamethasone, faster onset | Bradycardia, hypotension |
| Combined Dex-Dex | 4 mg + 25 µg | No clear superiority over dexamethasone alone | Off-label; obtain consent |
| Magnesium sulphate | 150 mg | Modest prolongation | Limited evidence (SAJAA 2022) |
- Continuous catheters (interscalene, costoclavicular, infraclavicular) enable ≥ 48 h analgesia at home (0.2 % ropivacaine 5–8 mL h⁻¹); provide rescue bolus protocol and emergency contact.
Complications & Mitigation
| Complication | Incidence | Prevention / Management |
|---|---|---|
| Haemidiaphragmatic paralysis | High with ISB | Use STB/CCB; limit LA volume ≤ 15 mL |
| Pneumothorax (SCB) | < 1 % with US | Visualise pleura; lateral probe orientation |
| LAST | 1: 10 000 | Dose calculation, incremental injection, aspiration, US, lipid kit ready |
| Nerve injury | < 0.2 % persistent | Avoid high opening pressure (> 15 psi), no motor twitch at < 0.3 mA |
| Haematoma/bleeding | ↑ with anticoagulants | Follow ASRA/SASA anticoagulation intervals |
Intravenous Regional Anaesthesia (Bier Block)
- LA: Prilocaine 0.5 % 3 mg kg⁻¹ (max 400 mg) or Lidocaine 0.5 % 1.5 mg kg⁻¹ (max 200 mg); no additives or adrenaline.
- Minimum tourniquet time 30 min; safe deflation technique–release 5 s, re-inflate 1 min, final release.
- Contra-indications: Sickle cell disease, severe peripheral vascular disease, infection, crush injury.
- Post-deflation: observe ≥ 20 min for LAST.
Block Performance & Monitoring
- Triple safety–real-time ultrasound + low-current nerve stimulation (≤ 0.5 mA, 0.1 ms) + Opening Injection Pressure (OIP) < 15 psi.
- Connect needle to nerve stimulator (0.5mA, 0.1msec, 2Hz)
- Advance needle towards the nerve or plexus
- Needle adequately placed as seen on US
- No twitch
- 1-2 mL injection of LA results in adequate spread in the desired tissue plane OIP normal <15psi
- Needle adequately placed as seen on US
- Twitch present
- Reposition the needle to assure NO twitch present at <0.5mA
- 1-2 mL injection of LA results in adequate spread in the desired tissue plane OIP normal <15psi
- Needle adequately placed as seen on US
- Complete injection
- No response:
- Increase current to 1.5mA
- Adjust needle placement by US
- Document volume, concentration, adjuvants, site, side, complications in the regional register (SASA QI requirement).
- Sedation: follow Procedural sedation guideline; full ASA monitoring if midazolam / propofol used.
Evidence
Use and Outcome Benefit
| Approach | Typical operations (proven benefit) | Representative evidence & key outcomes* |
|---|---|---|
| Interscalene (ISB) | Total shoulder arthroplasty, rotator-cuff repair, clavicle fixation | Meta-analysis of 14 RCTs (≈1200 pts, 2022) – pain scores ↓ > 3 cm Was for 24 h, IV morphine-equivalent ↓ 22 mg, earlier physiotherapy; but 94 % hemi-diaphragm paresis |
| Superior/Upper trunk | Shoulder arthroscopy, open Bankart repair | Systematic review 2023 – analgesia non-inferior to ISB with diaphragm paresis ↓ to ≈15 %, fewer dyspnoea events, earlier discharge |
| Supraclavicular (SCB) | Mid-humerus plate, elbow arthroplasty, radial-forearm free flap | RCT 2024 (n = 120)–success 98 %, opioid use first 12 h ↓ 40 % vs axillary; quicker onset than infraclavicular for elbow surgery; pneumothorax 0 % under ultrasound |
| Costoclavicular (CCB) | AV-fistula creation, distal humerus fixation, outpatient hand surgery catheters | BJA 2024 RCT–block success 100 %, diaphragm paresis 4 %, catheter dislodgement 2 % (vs 12 % infraclavicular), analgesia identical; cohort 2024 confirmed <10 % phrenic involvement |
| Infraclavicular (ICB) | Elbow, forearm, wrist surgery when complete tourniquet cover needed | Medicine 2024 meta-analysis–longer motor block and block duration than SCB; fewer paraesthesiae than SCB; similar surgical readiness time |
| Axillary | Carpal tunnel, metacarpal/phalangeal fixation, tendon repair | 2023 network meta-analysis–no difference in surgical anaesthesia vs SCB, but time-to-block longest; high patient satisfaction; musculocutaneous must be blocked separately |
| Distal single-nerve blocks (median, ulnar, radial, musculocutaneous) | Wrist arthroscopy, trigger-finger release, tendon transfers | RCT 2019–equivalent OR readiness and lower tourniquet pain vs SCB; preserves proximal motor, allows immediate elbow mobilisation |
| Intravenous regional anaesthesia (Bier) | Short (< 60 min) reduction / fixation, foreign-body removal | Prospective trial 2021–pain control equivalent to wide-awake local; shorter theatre time; but tourniquet discomfort limits > 90 min cases |
Practice Points
- Shoulder surgery–where respiratory compromise exists, superior trunk block or combined suprascapular + axillary blocks provide comparable analgesia with greatly reduced diaphragm impairment.
- Elbow and forearm–costoclavicular or infraclavicular blocks give faster readiness and more reliable tourniquet tolerance than axillary.
- Hand surgery day-case–axillary or distal blocks minimise motor block of proximal joints, facilitating same-day physiotherapy.
- Home catheters–costoclavicular catheters show lower dislodgement and superior patient-reported quality-of-recovery scores compared with interscalene catheters.
- IVRA remains the simplest technique for very short procedures but offers no post-operative analgesia; wide-awake local anaesthesia-no tourniquet (WALANT) may further reduce theatre time for carpal-tunnel release.
Safety & Outcome-linked Dosing
| LA concentration (single-shot) | Volume range | Target duration | Evidence-based comment |
|---|---|---|---|
| 0.5 % Ropivacaine | 10-15 mL (STB) / 15-25 mL (SCB/CCB) | 10-14 h | RCTs show no increase in LAST at ≤ 3 mg kg⁻¹ total |
| 0.5 % Levobupivacaine | 20-30 mL (ICB/Axillary) | 12-18 h | Longer motor block; preferred for prolonged tourniquet |
| 0.25 % Ropivacaine continuous catheter | 5-8 mL h⁻¹ | Up to 72 h | Cost–effective for day-case shoulder arthroplasty |
| 0.5 % Prilocaine (IVRA) | 3 mg kg⁻¹ (max 400 mg) | Up to 60 min | Failure rate < 3 % when 30-min cuff rule observed |
Complication Trends (Ultrasound era)
| Complication | Reported rate | Comment |
|---|---|---|
| LAST | 0.01 % upper-limb blocks; virtually zero in distal blocks | Relates directly to total mg injected; keep < 3 mg kg⁻¹ bupivacaine equivalents |
| Pneumothorax | 0–0.7 % SCB; none with CCB, ICB, distal | Use linear probe in coronal orientation and visualise pleura |
| Persistent neurological deficit | 0.2 % (all) | High opening-pressure injection triples risk |
| Diaphragmatic paresis | 94 % ISB, 15 % STB, < 10 % CCB/ICB | Consider patient comorbidities |
Nerve Injury After Peripheral Nerve Block–Recognition & Evidence-Based Pathway
Definition
- New pain, paraesthesia, numbness or motor weakness persisting > 48 h after the expected resolution of block (≈ 24 h for single-shot long-acting local anaesthetic).
- May be partial (sensory-only) or complete (sensorimotor).
Incidence of Nerve Injury After Peripheral Nerve Block
| Category of deficit | Operational definition | Best-estimate incidence |
|---|---|---|
| Permanent neurological deficit | Persistent sensorimotor symptoms ≥ 12 months | ≤ 0.04 % (≈ 1: 2 500 blocks) |
| Transient neuropraxia | New sensory ± motor deficit lasting > 7 days but resolving < 12 months | 0.8–2 % |
- Figures derived from large prospective registries (> 170 000 blocks) and multicentre observational studies published 2017-2024.
- Most injuries are neurapraxic and resolve within 12 weeks.
Principal Mechanisms
- Needle or catheter trauma (especially intrafascicular placement)
- High-pressure or intraneural injection causing ischaemia–reperfusion injury
- External compression–tourniquet, tight dressings, extreme positioning
- Surgical traction, haematoma, or oedema around the nerve
Immediate Actions (Day 0–1)
- Review records–block details, needle type, LA dose, surgical notes, tourniquet pressure/duration, anticoagulation.
- Focused neuro-examination–document dermatomal sensation, strength (Medical Research Council scale) and compare with contralateral limb.
- Escalate–inform operating surgeon, block anaesthetist and Acute Pain/Regional Team.
Algorithm
| Clinical picture | Key steps in first 48 h | Subsequent pathway |
|---|---|---|
| Mild, improving sensory symptoms | Reassure; optimise analgesia; provide patient information leaflet | Review in 2 weeks → if fully resolved, discharge; if persistent, proceed as for “sensory-only persistent” |
| Persistent sensory deficit at 2 weeks | Arrange outpatient neurophysiology at 3–4 weeks (NCS/EMG) | • If normal → reassure, physio, re-review 6–8 weeks • If abnormal → formal Neurology referral ± MRI |
| Any motor weakness or worsening deficit | Urgent imaging to exclude compressive lesion (US or MRI within 24 h); check platelet count & coagulation | • Haematoma/space-occupying lesion → surgical decompression • No SOL → same pathway as above but Neurology referral within 48 h |
| Severe pain out of proportion + motor deficit | Consider compartment syndrome; measure pressures; maintain normotension | Emergency fasciotomy if indicated |
- Timing rationale: meaningful EMG/NCS requires Wallerian degeneration (≈ 3 weeks). Earlier studies give false reassurance
Investigations
- Ultrasound (bedside)–detects haematoma, nerve swelling or transection.
- MRI neurography–delineates nerve continuity, oedema, scarring.
- Laboratory–CK, full blood count, INR if haematoma suspected.
Management
- Conservative–neuropathic analgesics (duloxetine, gabapentin), physiotherapy, occupational therapy, psychological support.
- Surgical–indicated for laceration, entrapment, enlarging haematoma or nerve sheath tumour. Early (< 3 months) neurolysis or grafting improves outcome.
- Documentation & Duty of Candour–explain events, expected course, planned follow-up; record in regional-block register and national incident system.
Follow-up Schedule
| Timepoint | Action |
|---|---|
| 48 h phone call | Reassess symptoms; reinforce advice |
| 2 weeks clinic | Repeat neuro-exam; triage investigations |
| 6–8 weeks | Review results; decide discharge vs ongoing care |
| ≥ 3 months | Refer to specialist nerve injury unit if no improvement |
Links
- Lower limb blocks
- Local anaesthetics
- Truncal blocks
- Anticoagulation and blocks
- Ortho regionals
- Shoulder surgery
References:
- Wai, C. L. W. and Irwin, M. G. (2012). Regional blocks in orthopaedics. Anaesthesia &Amp; Intensive Care Medicine, 13(3), 89-93. https://doi.org/10.1016/j.mpaic.2011.12.004
- Horlocker, T. T., Vandermeuelen, E., Kopp, S. L., Gogarten, W., Leffert, L., & Benzon, H. T. (2019). Regional anesthesia in the patient receiving antithrombotic or thrombolytic therapy: american society of regional anesthesia and pain medicine evidence-based guidelines (fourth edition). Obstetric Anesthesia Digest, 39(1), 28-29. https://doi.org/10.1097/01.aoa.0000552901.03545.fb
- Checketts, M. R. (2016). Intravenous regional anaesthesia. Anaesthesia &Amp; Intensive Care Medicine, 17(4), 192-193. https://doi.org/10.1016/j.mpaic.2015.12.013
- FRCA Mind Maps. (2024). Retrieved June 5, 2024, from https://www.frcamindmaps.org/
- Anesthesia Considerations. (2024). Retrieved June 5, 2024, from https://www.anesthesiaconsiderations.com/
- Boutique Workshops. (n.d.). In NYSORA. Retrieved June 26, 2024, from https://www.nysora.com/mec-category/boutique-workshops/
- ASRA Pain Medicine. (n.d.). Guidelines. Retrieved June 27, 2024, from https://www.asra.com/guidelines-articles/guidelines
- European Society of Regional Anaesthesia & Pain Therapy (ESRA). (n.d.). Guidelines. Retrieved June 27, 2024, from https://esraeurope.org/guidelines/
- Teaching videos
- Shen Y, et al. Ultrasound-guided costoclavicular vs supraclavicular block for upper-limb surgery: randomised trial. Br J Anaesth 2024;133:114-22.
- Abdallah FW, et al. Superior trunk block as a phrenic-sparing alternative to interscalene block: systematic review. Reg Anesth Pain Med 2023;48:375-84.
- Lee Y, et al. Diaphragm-sparing efficacy of costoclavicular block: prospective cohort study. Korean J Anesthesiol 2024;77:312-20.
- Pehora C, et al. Combined dexamethasone and dexmedetomidine for brachial plexus block: meta-analysis. Anesthesiology 2024;140:621-35
- Nienaber LN, et al. Ultrasound-guided brachial plexus block: SA experience. SAJAA 2022;28:180-6.
- Jurgens FX, et al. Magnesium sulphate as an adjuvant in SAP block: randomised study. SAJAA 2022;28:94-101.
- StatPearls. Intravenous Regional Anaesthesia (Bier Block). Updated 2024. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430760/
- Gray A, et al. Prilocaine vs lidocaine for Bier block: comparative study. Anaesth Intensive Ther 2024;56:88-95.
- Southern African Society of Anaesthesiologists. Guidelines for peripheral nerve blocks and local anaesthetic safety. Johannesburg; 2024.
- Neal JM, et al. ASRA Practice Advisory on neurologic complications associated with regional anaesthesia. Reg Anesth Pain Med 2023;48:455-64.
Summaries:
Superior trunk block
Suprascapular and axillary nerve block
Brachial plexus blocks
Elbow and wrist blocks
Copyright
© 2025 Francois Uys. All Rights Reserved.
id: “7bd5ffde-54eb-4d6c-a5db-5f0727748c8b”



