{}
Obstetric Emergencies
Obstetric Trauma
Introduction
- Always assume any woman of childbearing age with trauma may be pregnant until excluded by β-hCG assay or ultrasound.
- In South African series, 4% of female trauma admissions were pregnant; mechanisms: blunt 57%, penetrating 21%, burns 12%; 52% intentional, 26% road traffic accidents. Surgical intervention was required in 12%, with fetal loss in 80% of those cases. One-third of maternal traumas resulted in fetal demise, correlating with high maternal Injury Severity Scores.
Physiological and Anatomical Changes
Airway
- Pregnant patients have up to an eightfold increased risk of difficult or failed intubation due to airway oedema, weight gain and breast enlargement. Pre‑oxygenate with 100% O₂ and consider early use of videolaryngoscopy and smaller endotracheal tubes (e.g. 6.5–7.0 mm internal diameter).
Respiratory
- Oxygen consumption increases by 20–30% and functional residual capacity decreases by 20%, reducing apnoea tolerance. Aim for SpO₂ ≥ 95% with supplemental oxygen.
- Diaphragm is elevated by up to 4 cm; intercostal chest drain placement remains in the 4th or 5th intercostal space at the mid‑axillary line, preferably under ultrasound guidance.
Gastrointestinal
- Delayed gastric emptying and reduced lower oesophageal sphincter tone increase aspiration risk after 16 weeks’ gestation. Apply rapid‑sequence induction (RSI) principles.
Cardiovascular
- Plasma volume increases by 30–50%, but red cell mass by only 20–30%, creating physiological anaemia. Up to 30–35% blood loss may be occult before hypotension.
- After 20 weeks’ gestation, supine aortocaval compression can reduce venous return; position with left lateral tilt of 15° or perform manual left uterine displacement.
- Fetal distress may be an early indicator of maternal hypovolaemia. Secure two large‑bore (14–16 G) cannulae above the diaphragm; restrict vasopressor use to persistent hypotension after adequate volume resuscitation.
Haematology
- Pregnancy is a hypercoagulable state: increased fibrinogen, factors VII–X, reduced protein S. However, dilutional coagulopathy may occur with massive haemorrhage.
Radiological Considerations
- Do not delay maternal imaging for foetal concerns; radiation doses < 50 mGy carry negligible teratogenic risk. Foetal organogenesis is most susceptible between weeks 2–7.
- Use focused assessment with sonography in trauma (FAST) for maternal intra‑abdominal bleeding, and obstetric ultrasound for foetal viability and placental evaluation.
Foetal Monitoring
- Continuous cardiotocography (CTG) for at least 4–6 hours in viable pregnancies (> 24 weeks). Extend monitoring if uterine irritability, vaginal bleeding, ruptured membranes or significant maternal injury are present.
- Delay speculum or digital vaginal examination in active bleeding until placenta praevia or vasa praevia is excluded by imaging.
Foeto‑Maternal Haemorrhage
Allo‑immunisation
- Even 0.1 mL of Rh(D)-positive foetal blood can sensitise an Rh(D)-negative mother. Administer anti-D immunoglobulin 1500 IU (300 µg) within 72 hours of any Rho-positive foetal red cell exposure; calculate additional dose based on Kleihauer–Betke or flow cytometry quantification.
Fetal Anaemia
- Perform Kleihauer–Betke testing in all Rh(D)-negative women after significant blunt trauma; consider for symptomatic cases after 20 weeks’ gestation.
Blood Transfusion and Cell Salvage
-
Modern intraoperative cell salvage with leucocyte depletion filters effectively removes amniotic debris; discard autologous blood collected prior to delivery of placenta.
-
Use O negative blood if crossmatched units are unavailable. Target fibrinogen > 2 g L⁻¹ in major haemorrhage.
Ethical Considerations
Informed Consent
- Discuss risks of anaesthesia, radiological investigations and blood transfusion; obtain consent balancing maternal benefit and foetal risk.
Brain‑Dead Pregnant Patient
- Multidisciplinary management with obstetrics, anaesthesia, neonatology and ethics. Maintain somatic support until foetal maturity; delivery optimally by caesarean section.
Breech Presentation
Risks
- Maternal: increased operative morbidity, perineal trauma, postpartum haemorrhage.
- Foetal: preterm birth, birth trauma, cord prolapse, head entrapment, asphyxia.
Management
- External cephalic version at ≥ 36 weeks in low‑risk pregnancies under tocolysis and ultrasound guidance.
- Term vaginal breech delivery may be considered in selected cases with experienced team, after informed consent; refer to RCOG 2017 criteria.
Analgesia and Anaesthesia
- Early labour neuraxial analgesia (epidural) recommended. For vaginal breech, maintain adequate block to T10–S5; be prepared for rapid conversion to general anaesthesia.
- For caesarean section: neuraxial first-line; general anaesthesia with RSI if urgent.
- Uterine relaxation: intravenous nitroglycerin 50–200 µg bolus or 400–800 µg sublingual for head entrapment, followed by phenylephrine to maintain maternal blood pressure.
Category 1 Caesarean Section
- Defined as immediate threat to life of woman or foetus. Aim decision‑to‑delivery interval ≤ 30 minutes as a systems audit, not a rigid benchmark
Pre‑Theatre Interventions
- Position with left lateral tilt.
- 100% O₂ via face mask.
- Rapid crystalloid infusion (avoid dextrose).
- Consider tocolysis (e.g. terbutaline 250 µg subcutaneously) if hyperstimulation from oxytocin infusion complicates CTG.
Anaesthetic Technique
- RSI with cricoid pressure; preoxygenation ≥ 3 minutes.
- Rapid‑sequence spinal anaesthesia may be considered if no contraindications, with ‘no‑touch’ sterile technique and readiness to convert to GA.
Uterine Inversion
Recognition and Initial Management
- Presents with postpartum haemorrhage, hypovolaemic shock and uterine fundus palpable in the vagina.
- Call for obstetric and anaesthetic assistance; prepare massive transfusion protocol.
Tocolysis and Reduction
- Administer intravenous nitroglycerin 50–200 µg boluses (repeat as needed) or deep volatile anaesthesia following RSI to achieve uterine relaxation.
- Manoeuvre fundal replacement (Johnson method) immediately after tocolysis
Post‑Reduction Uterotonic Therapy
- Oxytocin 40 IU in 1 L crystalloid infusion or 100 µg carbetocin IV slow injection.
- Ergonovine 0.2 mg IM then 0.2 mg IV slow push.
- Carboprost trometamol 0.25 mg IM, repeat every 15 minutes up to 2 mg total.
- Misoprostol 800 µg per rectum.
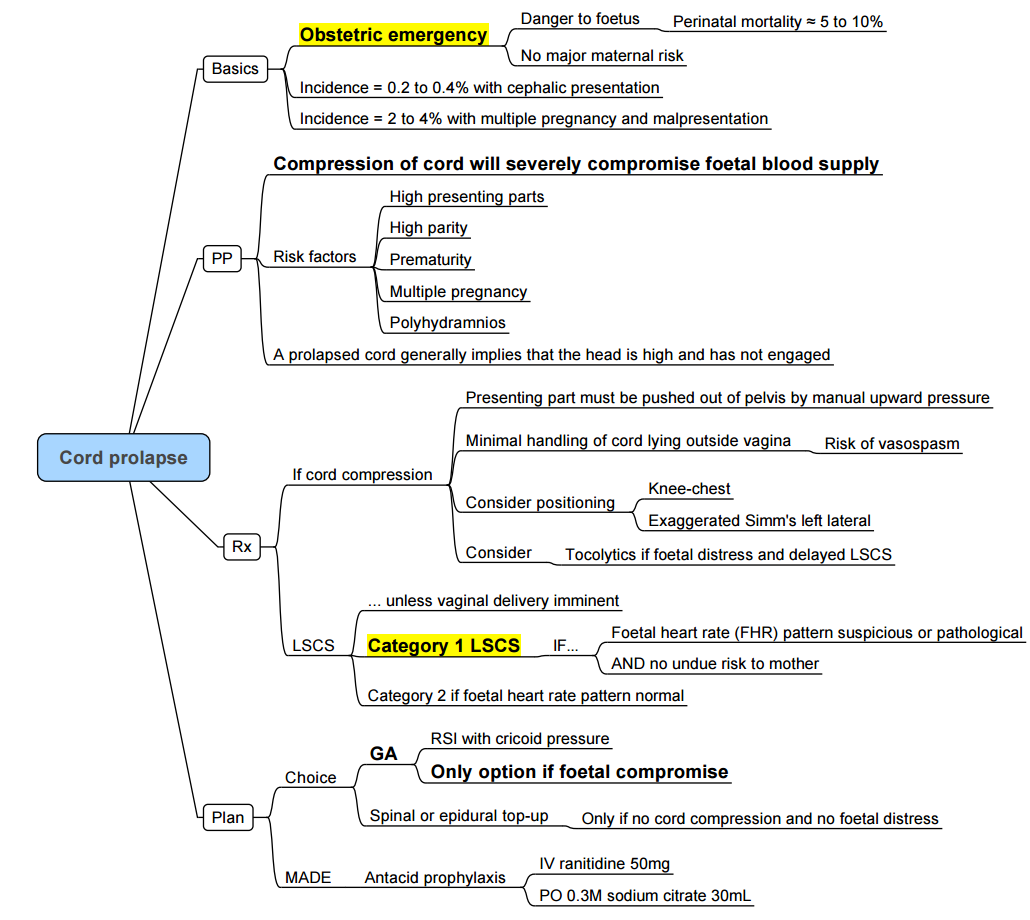
Cord Prolapse
Links
- Anaesthesia emergencies
- Amniotic fluid embolism and PE
- Maternal conditions
- Gynaecological Surgery
- Fetus and Placenta
- Non obstetric surgery
- Obstetric haemorrhage
- Maternal collapse and CPR
References:
- ACOG Practice Bulletin No. 198: Prevention of Rh D Alloimmunisation. Obstet Gynecol. 2018;132(1):e1–10.
- RCOG Green-top Guideline No. 20: The Management of Breech Presentation. London: RCOG; 2017.
- NAP4: Cook TM, et al. Severe complications of airway management in the UK: a national audit. Anaesthesia. 2011;66(5):317–45.
- Hofmeyr GJ, et al. Prevention of haemorrhage in obstetrics. Curr Opin Obstet Gynecol. 2016;28(6):.5. Smith I, et al. Ultrasound in trauma: advanced emergency medicine. Best Pract Res Clin Anaesthesiol. 2017;31(1):73–86.
- FRCA Mind Maps. (2024). Retrieved June 5, 2024, from https://www.frcamindmaps.org/
- Anesthesia Considerations. (2024). Retrieved June 5, 2024, from https://www.anesthesiaconsiderations.com/
- Richardson, A., Wittenberg, M., & Lucas, D. (2015). An urgent call to the labour ward. Continuing Education in Anaesthesia Critical Care &Amp; Pain, 15(1), 44-49. https://doi.org/10.1093/bjaceaccp/mku028
- Leta M, Assefa N, Tefera M. Obstetric emergencies and adverse maternal-perinatal outcomes in Ethiopia; A systematic review and meta-analysis. Front Glob Womens Health. 2022 Oct 26;3:942668. doi: 10.3389/fgwh.2022.942668. PMID: 36386434; PMCID: PMC9643843.
Summaries:
Obstetrics anaesthesia considerations
—
Copyright
© 2025 Francois Uys. All Rights Reserved.
id: “79214c91-6f3e-487b-8163-5e8b81aa94ef”



