- Physiology of One Lung Ventilation
- One Lung Anesthesia
- One Lung Ventilation
{}
Physiology of One Lung Ventilation
Thoracoscopy necessarily implies a derangement in physiology, whether the patient is awake and spontaneously breathing or anesthetized and paralyzed.
Spontaneous Breathing
- The basic physical driving force is the pressure gradient generated by the respiratory muscles, the elastic components of the chest wall, and the lungs between the alveolar pressure and the atmospheric pressure.
- This gradient results in airflow between the alveolar space and the outer environment, facilitating gas exchange in the alveoli.
- The pressure difference (gradient) is determined by the following universal equation:
- Pao + Pmus = PEEP + (Ers × V) + (Rrs × Flow)
- Where:
- Pao: Airway opening pressure
- Pmus: Muscle pressure
- PEEP: Positive end-expiratory pressure
- Ers: Elastance of the respiratory system
- V: Volume
- Rrs: Resistance of the respiratory system
- Flow: Flow rate
- Where:
Lateral Decubitus Position (LDP) Closed Chest
- Gravity (Vertical Gradient):
- Blood flow to the dependent lung is significantly greater than that to the nondependent lung.
- Vertical gradient in the pleural pressure increases ventilation relatively in the dependent lung.
- Lower Diaphragm Efficiency:
- The dome of the lower diaphragm is pushed higher into the chest than the dome of the upper diaphragm, making the lower diaphragm more sharply curved than the upper diaphragm.
- Dependent Lung Compliance:
- The dependent lung is on a less favorable part of the compliance curve
Awake, Open Chest, Spontaneous Breathing
-
Mediastinal Shift:
- Atmospheric pressure in the open cavity exceeds the negative pleural pressure in the dependent hemithorax.
- Imbalance of pressure on the two sides of the mediastinum causes a downward displacement of the mediastinum into the dependent thorax.
- Inspiration:
- Downward movement of the diaphragm increases the negative pressure in the dependent lung and further displaces the mediastinum into the dependent hemithorax.
- Expiration:
- The diaphragm of the dependent lung moves upwards.
- The pressure in the dependent hemithorax becomes relatively positive, pushing the mediastinum upward out of the dependent hemithorax.
- The tidal volume in the dependent lung decreases due to inspiratory displacement caused by mediastinal movement.
- Inspiration:
- Mediastinal shift can cause decreased venous return to the heart and sympathetic activation, resulting in a clinical picture similar to that of shock.
-
Paradoxical Breathing (Pendelluft):
- Pleural cavity exposure to atmospheric pressure causes the lung to collapse due to unopposed elastic recoil.
- During spontaneous ventilation with an open hemithorax, this lung collapse is accentuated during inspiration and the lung expands during expiration.
- The mechanism of paradoxical respiration is similar to that of mediastinal shift.
- Inspiration:
- Descent of the diaphragm on the closed-chest side causes gas to enter the closed-chest lung normally. Gas also enters the closed-chest lung from the open-chest lung, causing the open-chest lung to paradoxically reduce in size during inspiration.
- Expiration:
- The reverse occurs, with the closed-chest lung filling the open-chest lung, causing the open-chest lung to paradoxically expand during expiration.
- Inspiration:
-
Other Problems:
- Patient-ventilator asynchrony can potentiate lung injury by volutrauma and barotrauma. Cyclic opening of smaller airways may lead to atelectotrauma, regional atelectasis, and increased ventilation heterogeneity.
- Increased alveolo-capillary pressure gradient potentially leads to interstitial edema.
Anesthetized, Paralyzed, Open Chest
- Positive pressure ventilation (PPV) in the anesthetized, paralyzed, open-chested patient in the LDP can rectify mediastinal shift and paradoxical respiration that occur in the awake patient.
- Ventilation-Perfusion Mismatch Concern:
- Right-to-left transpulmonary shunt, normally 6-10%, increases to 20-30% during one-lung ventilation (OLV).
- Reduced arterial oxygen content, as a higher fraction of the cardiac output passes from right to left without gas exchange.
- Increased fraction of inhaled oxygen (FiO2) exerts a lower arterial oxygen content elevating effect as shunt fraction increases.
Summary Of One-Lung Ventilation Physiology
| Clinical Scenario | Key Physiological Changes | Main Problems |
|---|---|---|
| Spontaneous breathing, closed chest | – Diaphragm generates negative pressure – Gravity favours blood flow to dependent lung |
– Lower (dependent) lung may be less compliant – Risk of ventilation mismatch |
| Spontaneous breathing, open chest | – Atmospheric air enters open pleural space – Mediastinal shift during inspiration/expiration |
– Mediastinal movement impairs lung expansion – ↓ Tidal volume, ↓ venous return |
| Paradoxical breathing (Pendelluft) | – Air shifts between lungs instead of environment – Collapsed lung expands in expiration |
– Inefficient ventilation – Worsens oxygenation – Can mimic shock |
| Ventilated (paralyzed), open chest | – Positive pressure stabilizes mediastinum – More predictable lung inflation |
– Right-to-left shunt ↑ (20–30%) – Hypoxia risk despite 100% FiO₂ |
Pendelluft Explained Simply:
| Phase | What Happens |
|---|---|
| Inspiration | Diaphragm moves down → air flows into the dependent lung Some air also flows from non-dependent lung → dependent lung (→ open lung shrinks paradoxically) |
| Expiration | Air in dependent lung shifts back into the non-dependent lung → the collapsed lung re-expands paradoxically |
This gas shuttling between lungs (not with the outside world) is called Pendelluft.
Reasons for V/Q Mismatch
- Blood Flow:
- Dependent lung more perfused than the nondependent lung due to gravity.
- Ventilation:
- Ventilation is greater to the nondependent lung (gravity, open chest, and paralyzed condition).
- Dependent lung ventilation is poor due to reduced lung volume (FRC), compression by the mediastinum, abdominal contents, suboptimal positioning, poor mucociliary clearance, and absorption atelectasis caused by increased FiO2.
- Compliance Curve Shift:
- Dependent lung is on a less compliant curve, while the nondependent lung lies on an improved compliance curve.
V/Q Change Across Different Lung Regions
Ventilation and perfusion both increase towards dependent areas (lowest at the apex and highest at the base if standing) but increase at different rates, leading to different V/Q ratios across zones:
- Apex: Ventilation > Perfusion ⇒ V/Q > 1 ⇒ Dead space ⇒ Alveolar O2 higher and CO2 lower than normal, and vice versa for arterial.
- Base: Ventilation < Perfusion ⇒ V/Q < 1 ⇒ Shunting
Summary: V/Q Changes in the Lateral Decubitus Position
Dependent Lung
- Ventilation: Reduced
- Perfusion: Increased
- Pulmonary Blood Flow: 80%
Non-Dependent Lung
- Ventilation: Increased
- Perfusion: Reduced
- Pulmonary Blood Flow: 20%
Compensation (HPV)
- Pulmonary arterial vasoconstriction in response to low alveolar oxygen tension.
- In pulmonary artery smooth muscle cells (PASMCs), resting membrane potential is maintained by outward potassium current, inhibited in a hypoxic environment, leading to membrane depolarization and opening of calcium channels, resulting in elevated cytoplasmic Ca2+ levels and contraction of pulmonary arteries.
- HPV diverts blood from nondependent (nonventilated) lung fields to dependent areas in a fast-acting, biphasic manner.
- HPV activates seconds after the hypoxic stimulus, reaching maximum effect in minutes, helping to decrease transpulmonary right-to-left shunting, optimizing oxygen delivery, and restoring V/Q matching.
- HPV is reversible until vascular remodeling occurs. After short hypoxia (<20 min), HPV declines and PVR normalizes upon reoxygenation. After prolonged hypoxia, HPV persists for hours despite full reoxygenation, resulting in greater V/Q mismatch and larger alveolar-to-arterial O2 pressure gradient (A-PaO2).
- Adequate HPV minimizes perfusion of the dependent lung and optimizes the shunt. Attenuating HPV should be avoided as it is influenced by demographic parameters, medications, acid-base balance, lung disease, and lung expansion degree.
Postoperative Systemic Inflammatory Response (SIR)
- Changes in cellular defense and cytokine levels during SIR can affect the clinical picture. SIR period lasts around 3–12 days, impacting early postoperative morbidity and 30-day mortality.
- Reduced levels and functions of lymphocytes and NK cells cause diminished cellular defense ability, leading to postoperative pneumonia, wound infection, or other inflammatory responses.
- Postoperative pneumonia rates are 5% and 10%, and wound infection rates are 0.4% and 1% after VATS and open lobectomies, respectively.
- Postoperative morbidity is lower (5%) than in relaxed surgery cases (23%).
Physiological Hypoxemia in OLV
- Mismatched V/Q Relationship:
- Some perfusion remains in the unventilated lung, resulting in a shunt.
- Impaired hypoxic pulmonary vasoconstriction worsens the shunt.
- Reduction in Functional Residual Capacity (FRC):
- Due to the effects of anesthesia and the lateral decubitus position.
- Atelectasis in the Ventilated Dependent Lung:
- Secondary to compression by mediastinal weight and abdominal content.
- Permissive Hypercarbia and Respiratory Acidosis:
- Rapid dissociation of oxygen from hemoglobin (Bohr effect).
One Lung Anesthesia
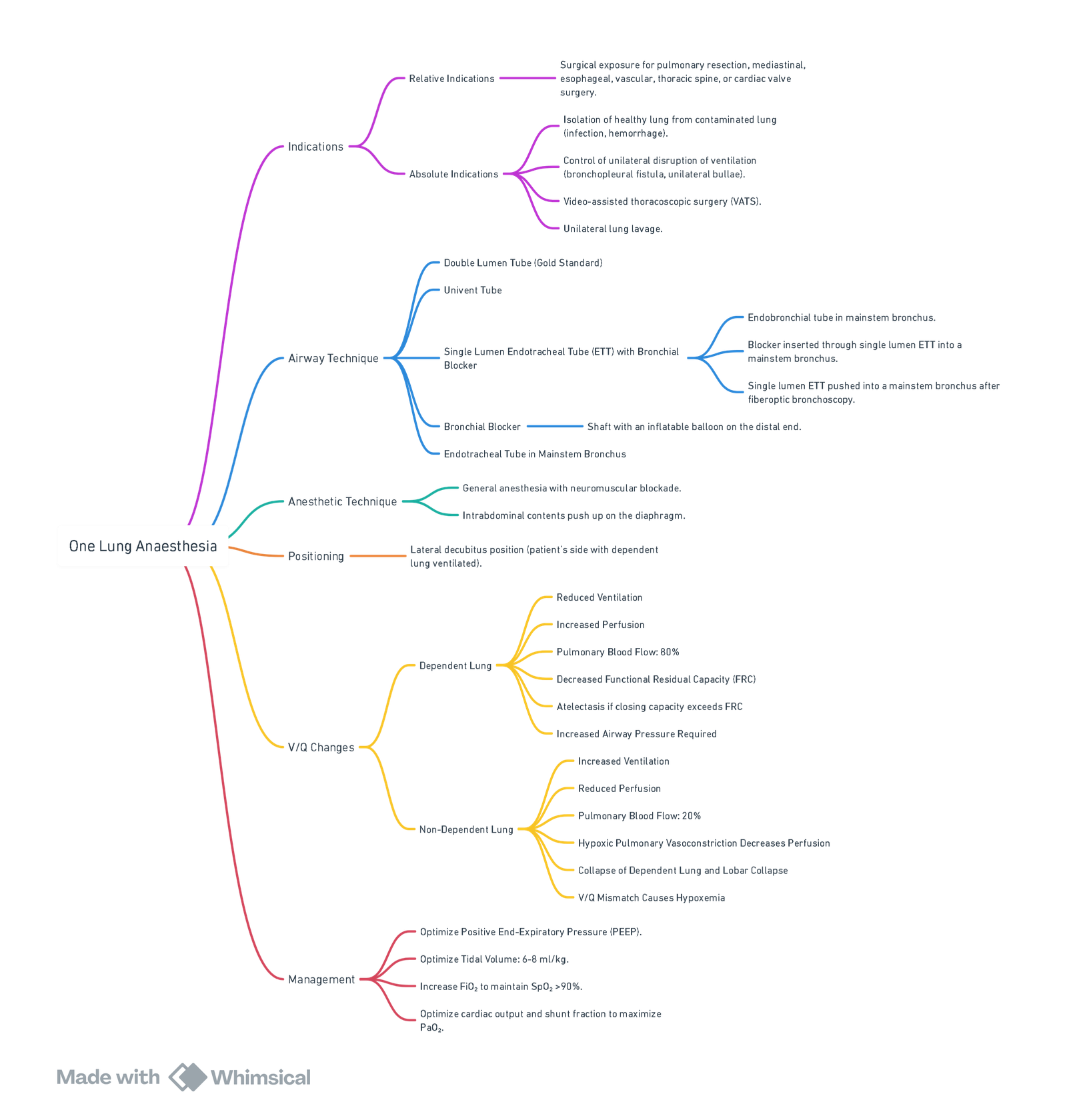
View or edit this diagram in Whimsical.
Preoperative Risk Assessment
Spirometry (post bronchodilator) and exercise data are used to predict the perioperative risk and postoperative respiratory reserve, i.e., pulmonary function and risk of respiratory failure. The predicted postoperative FEV1 (ppo FEV1) can be estimated from the formula using the total number of segments in both lungs (19: 9 in the left lung, 10 in the right lung) and the number of segments to be resected (y).
Risk Assessment for Surgical Suitability (PPO FEV₁ Calculation)
ppo FEV1 = FEV1 × ((19 − y) / 19)
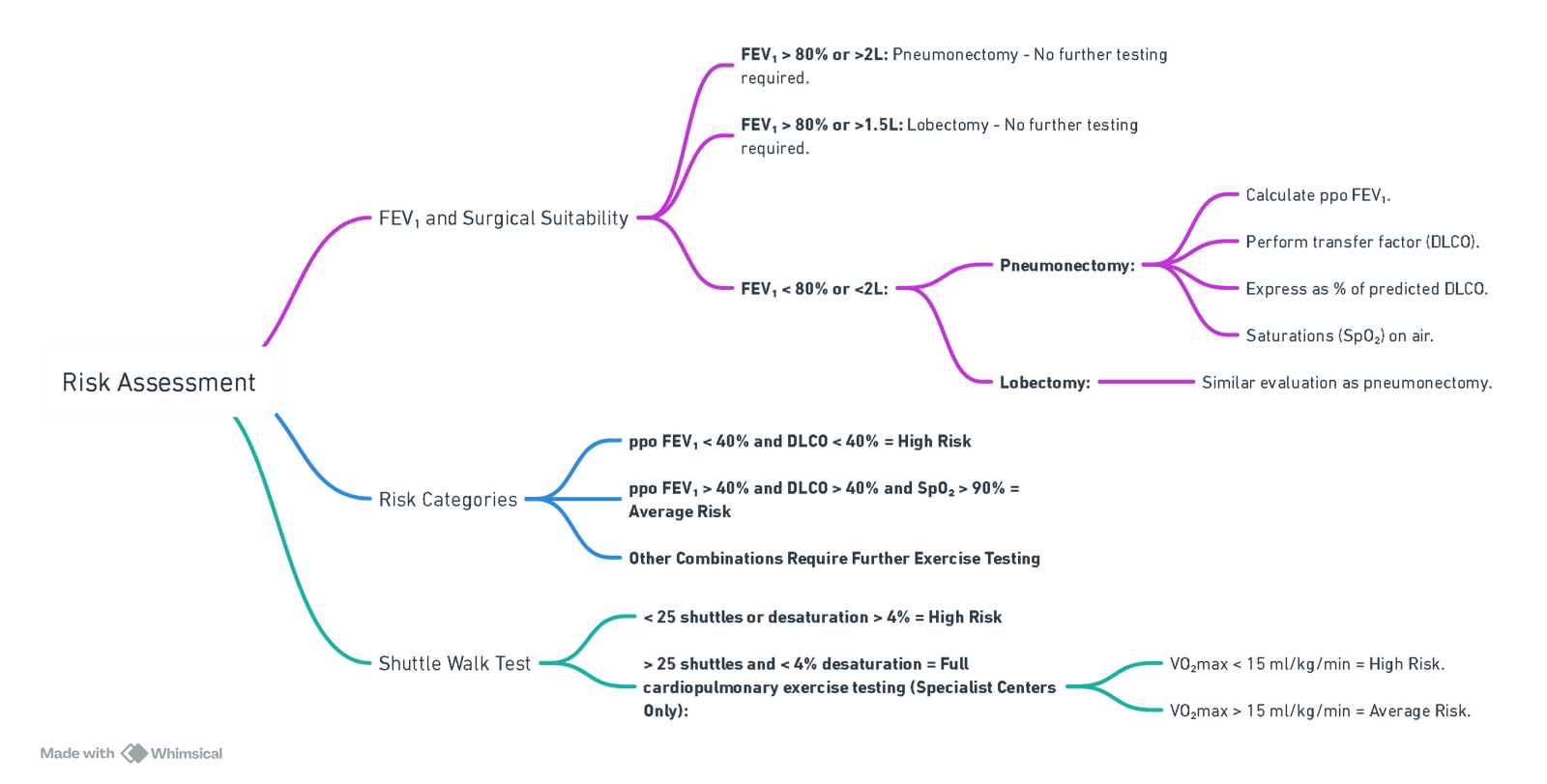
View or edit this diagram in Whimsical.
Factors Predicting Hypoxemia
- Low PO2 preoperatively.
- Ventilation of the left (smaller) lung.
- Supine position.
- Absence of reduced perfusion to areas of lung pathology (demonstrated on V/Q scan).
- Normal preoperative spirometry or restrictive lung disease.
Priority of Procedures for One-Lung Ventilation
High Priority:
- Prevention of Contamination of Healthy Lung:
- Infection.
- Hemorrhage.
- Control of Distribution of Ventilation:
- Bronchopleural fistula.
- Unilateral bullae.
- Airway disruption.
- Unilateral Lung Lavage
- Video-Assisted Thoracoscopic Surgery
Intermediate Priority:
- Higher Indication for Surgical Exposure:
- Thoracic aortic aneurysm repair.
- Pneumonectomy.
- Lung volume reduction.
- Minimally invasive cardiac surgery.
- Upper lobectomy.
- Lower Indication for Surgical Exposure:
- Esophageal surgery.
- Middle and lower lobectomy.
- Mediastinal mass resection.
- Bilateral sympathectomies.
There are four main indications for one-lung anesthesia: isolation of the lungs, improved surgical access, greater control over ventilation, and unilateral bronchopulmonary lavage.
One Lung Ventilation
- Creates an obligatory right-to-left transpulmonary shunt through the nonventilated nondependent lung.
- The nondependent lung is non-ventilated, and any blood flow to the non-ventilated lung becomes shunt flow, in addition to whatever shunt flow might exist in the dependent lung.
- Effect on PaO₂ and PaCO₂:
- PaO₂:
- Large alveolar-arterial oxygen tension difference and lower PaO₂.
- The ventilated lung cannot take up enough oxygen due to the flatness of the top end of the oxygen-hemoglobin dissociation curve, which does not allow for compensation for the nonventilated lung.
- PaCO₂:
- Less effect on PaCO₂.
- The ventilated lung can eliminate enough carbon dioxide to compensate for the nonventilated lung, keeping the alveolar carbon dioxide tension (PACO₂) to PaCO₂ gradients small.
- PaO₂:
- Compensation (Decrease Blood Flow to the Nondependent Lung):
- Passive Mechanisms: Gravity, surgical interference with the blood flow, and the extent of pre-existing disease in the nondependent lung.
- Active Vasoconstrictor Mechanism (HPV):
- The selective increase in the pulmonary vascular resistance of atelectatic lung diverts blood flow from the atelectatic lung toward the remaining normoxic or hyperoxic ventilated lung.
Physiological Changes of One Lung Ventilation
- Dependent lung (DL) is selectively ventilated.
- DL compressed by mediastinal contents → ↓ compliance and FRC → V/Q mismatching.
- DL receives 60% of blood.
- Non-dependent lung (NDL) still receives blood → shunt ← mitigated by HPV.
- Effect of drugs.
How to Collapse Lung
Passively:
- Diffusion hypoxia (FiO2 = 100%). Lung isolation. Access port = equilibration of intrapleural and atmospheric pressure = pneumothorax. Elastic recoil of the lung.
Actively:
- Introduction of CO2 into the pleural space. Rarely used except if a single ETT is used or to facilitate lung collapse with OLV.
Confirmation of Verres Needle if Capnothorax is Used to Collapse Lung
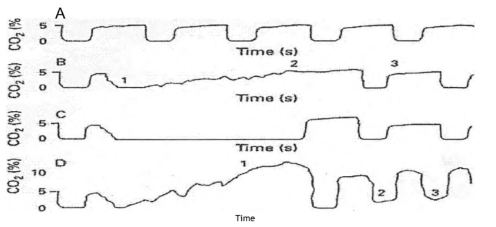
Definition
Capnothorax is a type of pneumothorax where carbon dioxide (CO₂) is present in the pleural cavity.
Etiology
Capnothorax is commonly associated with procedures such as laparoscopic surgery or any procedure involving insufflation of CO₂ into the pleural space.
Clinical Presentation and Diagnosis
The diagnosis of capnothorax can be suggested by changes in end-tidal CO₂ (EtCO₂) concentrations during ventilation. The scenarios below describe the potential changes observed during different conditions involving the placement of a Verres’ needle:
A. Normal Ventilation:
- Both lungs are ventilated normally.
- Expected EtCO₂: Stable, normal baseline values.
B. Correct Placement of Verres’ Needle in Intrapleural Space:
- Ventilation stops and the expiratory valve is opened to the atmosphere.
- Expired CO₂ drops to zero.
- 0.5 liters of CO₂ is insufflated through the Verres’ needle, partially collapsing the lung.
- Expired CO₂ concentration gradually returns to baseline (4-5%) as CO₂ diffuses and is expelled.
- Resumption of ventilation sees the waveform return to normal.
C. Verres’ Needle in Chest Wall or with Pleural Adhesions Preventing Lung Collapse:
- There is no increase in expired CO₂ concentration during insufflation.
- No significant change in EtCO₂ observed.
D. Lung Puncture with Verres Needle:
- During insufflation, expired concentration of CO₂ increases significantly.
- Resumption of ventilation does not return EtCO₂ to zero.
- Each successive ventilation shows an increase in EtCO₂.
Management
- Immediate cessation of CO₂ insufflation.
- Decompression of the pleural space if necessary.
- Monitoring and supportive care to manage any respiratory compromise.
- Thoracentesis may be required to evacuate CO₂ from the pleural space.
Complications
- Respiratory distress
- Hypoxemia
- Cardiovascular compromise
Drugs/Intervention And Physiological Effect
- Vasodilators (e.g., GTN, Dobutamine, β Agonists):
- Inhibit Hypoxic Pulmonary Vasoconstriction (HPV) – Increase Shunt.
- Vasoconstrictors (e.g., Metaraminol, Noradrenaline):
- Increase Shunt Due to Effects on Cardiac Output.
- Volatile Agents (e.g., Sevoflurane, Isoflurane, Desflurane):
- Attenuate HPV; Around 15-20% at 1 MAC for Isoflurane.
- Increase Pulmonary Vascular Resistance in Dependent Lung.
- Positive End-Expiratory Pressure (PEEP):
- Increase Shunt to Non-Dependent Lung.
- Fraction of Inspired Oxygen (FiO₂):
- High FiO₂ reduces vascular tone in non-diseased lung tissue and reduces shunt fraction.
Management of One-Lung Ventilation
- Higher FiO2 to keep SaO2 above 90%.
- The dependent lung should be ventilated with a tidal volume of approximately 6-10 ml/kg.
- The respiratory rate is then adjusted to maintain the PaCO2 at 40 mm Hg.
Troubleshooting
- Administer 100% oxygen.
- Confirm positioning with a fiberoptic bronchoscope.
- Check ventilator, circuit, and catheter mount.
- Clear secretions and debris by suctioning the dependent lung.
- Apply CPAP or entrain oxygen to the non-dependent lung by differential-lung positive end-expiratory pressure (PEEP) or continuous positive airway pressure (CPAP), or both.
- CPAP of 5-10 cm H2O to the nonventilated, nondependent lung.
- PEEP of 5-10 cm H2O to the dependent, ventilated lung (may cause an increase, no change, or a decrease in oxygenation and, therefore, is not a first-line maneuver by itself).
- If hypoxemia persists, then increase CPAP in the nondependent lung by 5 cm H2O increments, followed by increments in the dependent lung if necessary.
- Revert to two-lung ventilation.
- Clamp non-dependent pulmonary artery.
Differential-Lung Ventilation
- Low levels of positive pressure can be selectively and statically applied to only the nonventilated, nondependent lung. The application of CPAP to only the nonventilated lung substantially increases oxygenation.
- Low levels of CPAP maintain the patency of the nondependent lung airways, allowing some oxygen distention of the gas-exchanging alveolar space in the nondependent lung without considerably affecting the pulmonary vasculature.
- The single most efficacious maneuver to increase PaO2 during one-lung ventilation is to apply 5 to 10 cm H2O of CPAP to the nondependent lung.
- Because the volume of the ventilated dependent lung is often decreased during one-lung ventilation, attempts have been made to improve oxygenation by selectively treating the ventilated lung with PEEP.
- An accepted risk of selective dependent-lung PEEP is that the PEEP-induced increase in lung volume can cause compression of the small dependent-lung intra-alveolar vessels and increase dependent-lung pulmonary vascular resistance. Blood flow would then be diverted from the ventilated lung to the nonventilated lung, increasing the shunt and decreasing PaO2.
- Therefore, the effect of dependent-lung PEEP on arterial oxygenation is a trade-off between the positive effect of increasing the dependent lung functional residual capacity (FRC) and the V/Q ratio, and the negative effect of increasing the dependent-lung vascular resistance and shunting blood flow to the nonventilated lung.
- Dependent-lung PEEP may cause an increase, no change, or a decrease in oxygenation and, therefore, is not a first-line maneuver by itself. If oxygenation does not improve with 5 to 10 cm H2O of CPAP delivered to the nondependent lung, 5 to 10 cm H2O of PEEP should then be added to the dependent lung. If severe hypoxemia persists, then the nondependent-lung CPAP is increased to 10 to 15 cm H2O. If arterial oxygenation is still not satisfactory, then the dependent-lung PEEP is also increased to 10 to 15 cm H2O. In this way, a differential-lung PEEP and CPAP search for the maximum compliance and minimum right-to-left transpulmonary shunt is made in an attempt to find the optimal end-expiratory pressure for each lung and the patient as a whole.
- The resumption of two-lung ventilation is the fastest way to improve oxygenation. There should be no hesitation to ventilate the nondependent lung when severe hypoxemia persists.
Practicalities of One-Lung Ventilation (OLV)
- Increase FiO₂ to 100% before initiating OLV.
- Titrate O₂ down according to patient tolerance.
- Aim for peak pressures < 25-30 cmH₂O.
- Modify respiratory rate to avoid excessive hypercapnia.
- Pressure control ventilation (PCV) often results in lower peak pressures.
- Apply PEEP 5-10 cmH₂O, avoiding excessive levels to prevent worsening shunt.
Step-Wise Management of Hypoxia in OLV
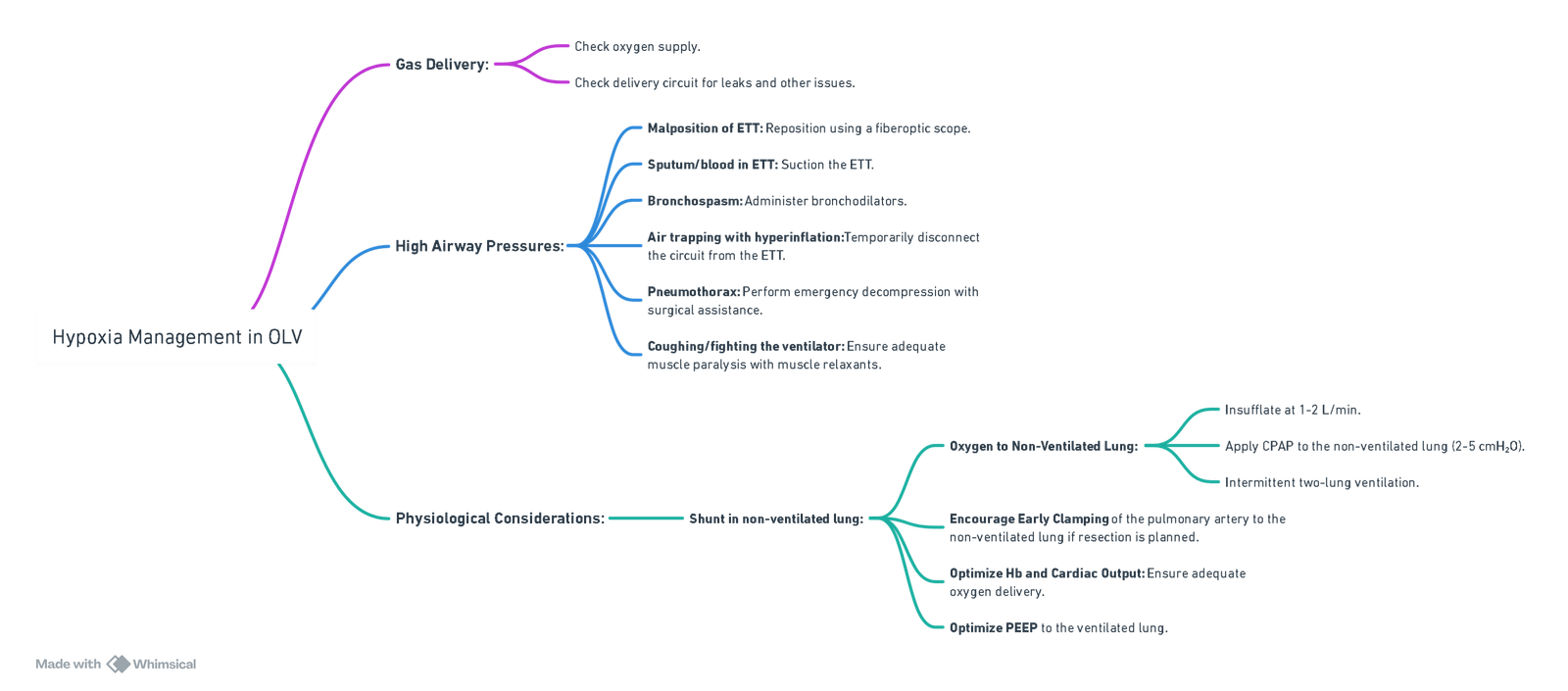
View or edit this diagram in Whimsical.
Complications of Video-Assisted Thoracoscopic Surgery (VATS)
- Atrial fibrillation: 10%
- Air leak: 7.2%
- Pneumonia: 2%
- Respiratory failure: 2%
- Empyema: 1.3%
- Deep vein thrombosis: 0.7%
- Bleeding: Rare but can be severe; ensure wide bore IV access.
One Lung Ventilation VIVA
Key Considerations
- Fresh tracheostomy: Anticipate difficult airway and altered anatomy.
- One-lung ventilation (OLV): Required for surgical exposure and lung isolation.
- Neuroprotection: Important in patients with concurrent neurological pathology.
- Other injuries: Perform a thorough trauma assessment; exclude head, spinal, or abdominal injuries.
Methods for Achieving One-Lung Ventilation
- Bronchial Blockers: Arndt blocker or EZ blocker as flexible options for selective lung isolation.
- Endobronchial intubation: Advance a single-lumen ETT into the right main bronchus under fibreoptic guidance.
- Double-Lumen Tube (DLT): Gold standard; insert orally and confirm placement with a fibreoptic bronchoscope.
- Hybrid techniques: e.g., combining fibreoptic scope with bronchial blocker for precise placement
Management of Intraoperative Hypoxaemia During OLV
- Initial Steps:
- Administer 100% FiO₂.
- Suction the operative (non-ventilated) lung.
- Check for circuit disconnections, leaks, kinks, or secretions.
- Confirm correct positioning of the DLT or bronchial blocker.
- Optimise Ventilation and Perfusion
- Minimise volatile agent (<1 MAC).
- Optimise cardiac output.
- Perform a recruitment manoeuvre on the ventilated lung (transient desaturation expected).
- Apply PEEP (5 cmH₂O) to the ventilated lung.
- Consider CPAP (1–2 cmH₂O) to the non-ventilated lung (recruit before applying CPAP; discuss with surgeon).
- Further Interventions:
- Revert to two-lung ventilation intermittently if needed.
- Consider partial ventilation techniques:
- Continuous oxygen insufflation.
- Selective lobar insufflation.
- Discuss surgical techniques to clamp pulmonary artery of the non-ventilated lung to reduce shunt.
Ventilation-Perfusion (V/Q) Mismatch in Lateral Position
- In lateral decubitus:
- Dependent lung: ↑ perfusion due to gravity.
- Non-dependent lung: ↑ ventilation.
- Results in V/Q mismatch.
- Hypoxic Pulmonary Vasoconstriction (HPV):
- Key protective mechanism to divert blood away from hypoxic alveoli.
- OLV-induced complications:
- Decreased ventilated lung surface: Due to mediastinal compression, cephalad diaphragm shift, and poor compliance.
- ↑ Ventilatory pressures in dependent lung: May impede perfusion and exacerbate shunting.
- Poor ventilation strategies: High tidal volumes or pressures risk lung injury.
Neuroprotective Strategies
- Maintain high-normal PaO₂: Be cautious of desaturation during OLV.
- Maintain normal–low PaCO₂: Permissive hypercapnia may be necessary but avoid excessive CO₂ to reduce risk of raised ICP.
- Head-up positioning: Often not feasible intraoperatively, but ideal for cerebral perfusion; consider alternatives to reduce intracranial pressure.
Links
- Respiratory physiology and Thoracic anaesthesia
- Double lumen and Bronchial blocker
- Whole lung lavage
- Open chest and Empyema
- Long volume reduction surgery
- Hypoxia Pulmonary Vasoconstriction (HPV)
Past Exam Questions
Anaesthetic Management for Bilateral Sympathectomy via VATS
A young healthy patient with hyperhidrosis presents for a bilateral sympathectomy through a video-assisted thoracoscopy. Defend your choice of patient management under the following headings:
a) Anaesthetic technique. (5)
b) Post-operative pain management. (3)
c) Appropriateness of this case in a day surgery setting. (2)
One Lung Ventilation
a) List the main causes of hypoxia during one-lung ventilation. (5)
b) List strategies that can be used to treat hypoxia during one-lung ventilation. (5)
Lung Isolation for Thoracic Surgery
A 59-year-old male is booked for the resection of the upper right lung lobe. The surgeon requests
that you provide lung isolation to facilitate the surgery
a) Name and briefly describe three lung isolation techniques applicable to this scenario. (6)
b) The patient develops hypoxaemia and the airway pressures increase significantly 15 minutes after the start of one-lung ventilation. Name two possible causes of hypoxaemia in this context and what action you will take to address each cause. (4)
References:
- Szabó, Z., Fabó, C., Oszlanyi, A., Hawchar, F., Géczi, T., Lantos, J., … & Furák, J. (2022). Anesthetic (r)evolution from the conventional concept to the minimally invasive techniques in thoracic surgery—narrative review. Journal of Thoracic Disease, 14(8), 3045-3060. https://doi.org/10.21037/jtd-22-80
- Jeffrey L. Horswell, Anesthetic techniques for thoracoscopy, The Annals of Thoracic Surgery, Volume 56, Issue 3, 1993, Pages 624-629, ISSN 0003-4975, https://doi.org/10.1016/0003-4975(93)90932-8.
- FRCA Mind Maps. (2024). Retrieved June 5, 2024, from https://www.frcamindmaps.org/
- Anesthesia Considerations. (2024). Retrieved June 5, 2024, from https://www.anesthesiaconsiderations.com/
Summaries:
Thoracic anaesthesia
OLV videos
Copyright
© 2025 Francois Uys. All Rights Reserved.
id: “e6320a95-bf58-4023-a1f3-d8e2f24178b2”



